| From | AVAC <[email protected]> |
| Subject | COVID News Brief: The news you need to know |
| Date | August 4, 2022 5:11 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
View this email in your browser ([link removed])
AVAC's weekly COVID News Brief provides a curated perspective on what COVID news is worth your time.
"It would be wrong for anyone to carry the stigma and weight of a social disease by himself. We all share the responsibility of life on a planet with viruses. But those of us living without the most lethal types of them must shoulder the responsibility more. The media heap a tremendous weight on people living with disease, whether it be COVID, AIDS, or monkeypox, making them feel like they’re a burden or some kind of individual failure—and the toll of this can be deadly."
—Steven Thrasher in The Atlantic ([link removed])
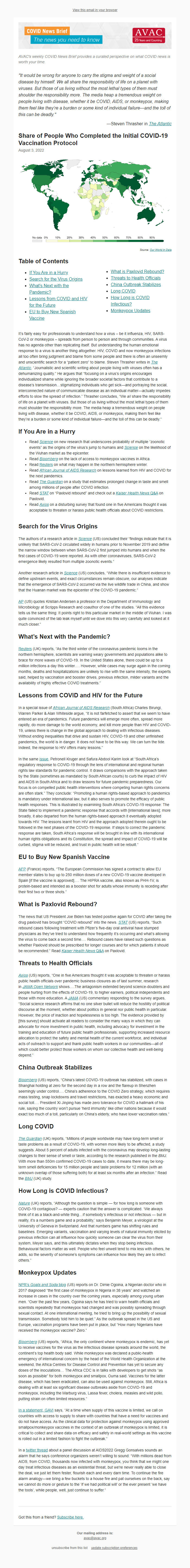
** Share of People Who Completed the Initial COVID-19 Vaccination Protocol
------------------------------------------------------------
August 3, 2022
Source: Our World in Data ([link removed])
** Table of Contents
------------------------------------------------------------
* If You Are in a Hurry (#hurry)
* Search for the Virus Origins (#origins)
* What’s Next with the Pandemic? (#next)
* Lessons from COVID and HIV for the Future (#lessons)
* EU to Buy New Spanish Vaccine (#spanish)
* What is Paxlovid Rebound? (#rebound)
* Threats to Health Officials (#threat)
* China Outbreak Stabilizes (#china)
* Long COVID (#long)
* How Long is COVID Infectious? (#infect)
* Monkeypox Updates (#pox)
It’s fairly easy for professionals to understand how a virus – be it influenza, HIV, SARS-CoV-2 or monkeypox – spreads from person to person and through communities. A virus has no agenda other than replicating itself. But understanding the human emotional response to a virus is another thing altogether. HIV, COVID and now monkeypox infections all too often bring judgment and blame from some people and there is often an unseemly and unscientific search for a “patient zero” to blame. Steven Thrasher writes in The Atlantic ([link removed]) , “Journalistic and scientific writing about people living with viruses often has a dehumanizing quality.” He argues that “focusing on a virus’s origins encourages individualized shame while ignoring the broader societal factors that contribute to a disease’s transmission…stigmatizing individuals who get sick—and portraying the social, interconnected nature of communicabl
e disease as an individual matter—actually impedes efforts to slow the spread of infection.” Thrasher concludes, “We all share the responsibility of life on a planet with viruses. But those of us living without the most lethal types of them must shoulder the responsibility more. The media heap a tremendous weight on people living with disease, whether it be COVID, AIDS, or monkeypox, making them feel like they’re a burden or some kind of individual failure—and the toll of this can be deadly.”
** If You Are in a Hurry
------------------------------------------------------------
* Read Science ([link removed]) on new research that underscores probability of multiple “zoonotic events” as the origins of the virus’s jump to humans and Science ([link removed]) on the likelihood of the Wuhan market as the epicenter.
* Read Bloomberg ([link removed]) on the lack of access to monkeypox vaccines in Africa.
* Read Reuters ([link removed]) on what may happen in the northern hemisphere winter.
* Read African Journal of AIDS Research ([link removed]) on lessons learned from HIV and COVID for the next pandemics.
* Read The Guardian ([link removed]) on a study that estimates prolonged change in taste and smell among millions of people after COVID infection.
* Read STAT ([link removed]) on “Paxlovid rebound” and check out a Kaiser Health News Q&A ([link removed]) on Paxlovid.
* Read Axios ([link removed]) on a disturbing survey that found one in five Americans thought it was acceptable to threaten or harass public health officials about COVID restrictions.
** Search for the Virus Origins
------------------------------------------------------------
The authors of a research article in Science ([link removed]) (US) concluded their “findings indicate that it is unlikely that SARS-CoV-2 circulated widely in humans prior to November 2019 and define the narrow window between when SARS-CoV-2 first jumped into humans and when the first cases of COVID-19 were reported. As with other coronaviruses, SARS-CoV-2 emergence likely resulted from multiple zoonotic events.”
Another research article in Science ([link removed]) (US) concludes, “While there is insufficient evidence to define upstream events, and exact circumstances remain obscure, our analyses indicate that the emergence of SARS-CoV-2 occurred via the live wildlife trade in China, and show that the Huanan market was the epicenter of the COVID-19 pandemic.”
AP ([link removed]) (US) quotes Kristian Andersen a professor in the Department of Immunology and Microbiology at Scripps Research and coauthor of one of the studies. “All this evidence tells us the same thing: It points right to this particular market in the middle of Wuhan. I was quite convinced of the lab leak myself until we dove into this very carefully and looked at it much closer.”
** What’s Next with the Pandemic?
------------------------------------------------------------
Reuters ([link removed]) (UK) reports, “As the third winter of the coronavirus pandemic looms in the northern hemisphere, scientists are warning weary governments and populations alike to brace for more waves of COVID-19. In the United States alone, there could be up to a million infections a day this winter…. However, while cases may surge again in the coming months, deaths and hospitalizations are unlikely to rise with the same intensity, the experts said, helped by vaccination and booster drives, previous infection, milder variants and the availability of highly effective COVID treatments.”
** Lessons from COVID and HIV for the Future
------------------------------------------------------------
In a special issue of African Journal of AIDS Research ([link removed]) (South Africa) Charles Birungi, Warren Parker & Alan Whiteside argue, “It is not farfetched to assert that we seem to have entered an era of pandemics. Future pandemics will emerge more often, spread more rapidly, do more damage to the world economy, and kill more people than HIV and COVID-19, unless there is change in the global approach to dealing with infectious diseases. Without ending inequalities that drive and sustain HIV, COVID-19 and other unfinished pandemics, the world is in danger. It does not have to be this way. We can turn the tide. Indeed, the response to HIV offers many lessons.”
In the same issue ([link removed]) , Petronell Kruger and Safura Abdool Karim look at “South Africa’s regulatory response to COVID-19 through the lens of international and regional human rights law standards for pandemic control. It draws comparisons with the approach taken by the State (sometimes as mandated by South African courts) to curb the impact of HIV and AIDS in South Africa and to draw lessons for future pandemic preparedness. Our focus is on compelled public health interventions where competing human rights concerns are often stark.” They conclude: “Promoting a human rights-based approach to pandemics is mandatory under international law, but it also serves to promote the efficacy of public health responses. This is illustrated by examining South Africa’s COVID-19 response: The State failed to implement a pandemic response that accords with [international laws]; more broadly, it also departed from the human
rights-based approach it eventually adopted towards HIV. The lessons learnt from HIV and the approach adopted therein ought to be followed in the next phases of the COVID-19 response. If steps to correct the pandemic response are taken, South Africa’s response will be brought in line with its international human rights obligations and its Constitution, the spread and impact of COVID-19 will be curbed, stigma will be reduced, and trust in public health will be rebuilt.”
** EU to Buy New Spanish Vaccine
------------------------------------------------------------
AFP ([link removed]) (France) reports, “The European Commission has signed a contract to allow EU member states to buy up to 250 million doses of a new COVID-19 vaccine developed in Spain [if the vaccine is approved]…. The HIPRA vaccine, also known as PHH-1V, is protein-based and intended as a booster shot for adults whose immunity is receding after their first two or three shots.”
** What is Paxlovid Rebound?
------------------------------------------------------------
The news that US President Joe Biden has tested positive again for COVID after taking the drug paxlovid has brought “COVID rebound” into the news. STAT ([link removed]) (US) reports, “Such rebound cases following treatment with Pfizer’s five-day oral antiviral have stumped physicians as they’ve tried to understand how frequently it’s occurring and what’s allowing the virus to come back a second time…. Rebound cases have raised such questions as whether Paxlovid should be prescribed for longer courses and for which patients it should be recommended.” Read Kaiser Health News ([link removed]) Q&A ([link removed]) on Paxlovid.
** Threats to Health Officials
------------------------------------------------------------
Axios ([link removed]) (US) reports, “One in five Americans thought it was acceptable to threaten or harass public health officials over pandemic business closures as of last summer, research in JAMA Open Network ([link removed]) shows….The antagonism extended beyond science-doubters and people hurting from the effects of COVID-19, to higher earners, political independents and those with more education. A JAMA ([link removed]) (US) commentary responding to the survey argues, “Social science research affirms that no one silver bullet will reduce the hostility of political discourse at the moment, whether about politics in general nor public health in particular. However, the price of inaction and hopelessness is too high. The evidence provided by [this survey] should activate all readers to consider the many ways
in which they can advocate for more investment in public health, including advocacy for investment in the training and education of future public health professionals, supporting increased resource allocation to protect the safety and mental health of the current workforce, and individual acts of outreach to support and thank public health workers in our communities—all of which could better protect those workers on whom our collective health and well-being depend.”
** China Outbreak Stabilizes
------------------------------------------------------------
Bloomberg ([link removed]) (US) reports, “China’s latest COVID-19 outbreak has stabilized, with cases in Shanghai holding at zero for the second day in a row and the flareup in Shenzhen seemingly under control…. China’s adherence to the COVID Zero strategy, which requires mass testing, snap lockdowns and travel restrictions, has exacted a heavy economic and social toll…. President Xi Jinping has made zero tolerance for COVID a hallmark of his rule, saying the country won’t pursue ‘herd immunity’ like other nations because it would exact too much of a toll, particularly on China’s elderly, who have lower vaccination rates.”
** Long COVID
------------------------------------------------------------
The Guardian ([link removed]) (UK) reports, “Millions of people worldwide may have long-term smell or taste problems as a result of COVID-19, with women more likely to be affected, a study suggests. About 5 percent of adults infected with the coronavirus may develop long-lasting changes to their sense of smell or taste, according to the research published in the BMJ. With more than 550m confirmed COVID-19 cases to date, it means there may be long-term smell deficiencies for 15 million people and taste problems for 12 million (with an unknown overlap of those suffering both) for at least six months after an infection.” Read the BMJ ([link removed]) (UK) study.
** How Long is COVID Infectious?
------------------------------------------------------------
Nature ([link removed]) (UK) reports, “Although the question is simple — for how long is someone with COVID-19 contagious? — experts caution that the answer is complicated. ‘We always think of it as a black-and-white thing…if somebody’s infectious or not infectious — but in reality, it’s a numbers game and a probability,’ says Benjamin Meyer, a virologist at the University of Geneva in Switzerland. And that numbers game has shifting rules and baselines. Emerging variants, vaccination and varying levels of natural immunity elicited by previous infection can all influence how quickly someone can clear the virus from their system, Meyer says, and this ultimately dictates when they stop being infectious. Behavioural factors matter as well. People who feel unwell tend to mix less with others, he adds, so the severity of someone’s symptoms can influence how likely they are to infect others.”
** Monkeypox Updates
------------------------------------------------------------
NPR’s Goats and Soda blog ([link removed]) (US) reports on Dr. Dimie Ogoina, a Nigerian doctor who in 2017 diagnosed “the first case of monkeypox in Nigeria in 38 years” and watched an increase in cases in the country over the coming years, especially among young urban men. “Over the past few years, Ogoina says he has tried to warn health officials and scientists repeatedly that monkeypox had changed and was possibly spreading through sexual contact. At one international meeting, he tried to bring up the possibility of sexual transmission. Somebody told him to be quiet.” As the outbreak spread in the US and Europe, vaccination programs have been put in place, but “How many Nigerians have received the monkeypox vaccine? Zero.”
Bloomberg ([link removed]) (US) reports, “Africa, the only continent where monkeypox is endemic, has yet to receive vaccines for the virus as the infectious disease spreads around the world, the continent’s top health body said. While monkeypox was declared a public-health emergency of international concern by the head of the World Health Organization at the weekend, the Africa Centres for Disease Control and Prevention has yet to secure any doses of the inoculations… The Africa CDC is in talks with developers to get shots “as soon as possible” for both monkeypox and smallpox, Ouma said. Vaccines for the latter disease, which has been eradicated, can also be used against monkeypox. Still, Africa is dealing with at least six significant disease outbreaks aside from COVID-19 and monkeypox, including the Marburg virus, Lassa fever, cholera, measles and wild polio, putting strain on often limited
resources.”
In a statement, GAVI ([link removed]) says, “At a time when supply of this vaccine is limited, we call on countries with access to supply to share with countries that have a need for vaccines and do not have access. As the clinical data for protection against monkeypox using approved smallpox/monkeypox vaccines in the context of an outbreak of monkeypox is limited, it is critical to collect and share data on efficacy and safety in real-world settings as this vaccine is rolled out in a limited fashion to fight the outbreak.”
In a twitter thread ([link removed]) about a panel discussion at AIDS2022 Gregg Gonsalves sounds an alarm that he says conference organizers weren’t willing to sound: “With millions dead from AIDS, from COVID, thousands now infected with monkeypox, you think that we might one day treat infectious diseases as an existential threat, but we're never really able to close the deal, we just let them fester, flourish each and every darn time. To continue the fire alarm analogy—we bring a few buckets to a house fire and pat ourselves on the back, say we cannot do more or gesture to the ‘if we had political will’ or the ever present ‘we have the tools’, while people, well, just continue to suffer.”
Got this from a friend? Subscribe here. ([link removed])
============================================================
Our mailing address is:
** [email protected] (mailto:[email protected])
** unsubscribe from this list ([link removed])
** update subscription preferences ([link removed])
AVAC's weekly COVID News Brief provides a curated perspective on what COVID news is worth your time.
"It would be wrong for anyone to carry the stigma and weight of a social disease by himself. We all share the responsibility of life on a planet with viruses. But those of us living without the most lethal types of them must shoulder the responsibility more. The media heap a tremendous weight on people living with disease, whether it be COVID, AIDS, or monkeypox, making them feel like they’re a burden or some kind of individual failure—and the toll of this can be deadly."
—Steven Thrasher in The Atlantic ([link removed])
** Share of People Who Completed the Initial COVID-19 Vaccination Protocol
------------------------------------------------------------
August 3, 2022
Source: Our World in Data ([link removed])
** Table of Contents
------------------------------------------------------------
* If You Are in a Hurry (#hurry)
* Search for the Virus Origins (#origins)
* What’s Next with the Pandemic? (#next)
* Lessons from COVID and HIV for the Future (#lessons)
* EU to Buy New Spanish Vaccine (#spanish)
* What is Paxlovid Rebound? (#rebound)
* Threats to Health Officials (#threat)
* China Outbreak Stabilizes (#china)
* Long COVID (#long)
* How Long is COVID Infectious? (#infect)
* Monkeypox Updates (#pox)
It’s fairly easy for professionals to understand how a virus – be it influenza, HIV, SARS-CoV-2 or monkeypox – spreads from person to person and through communities. A virus has no agenda other than replicating itself. But understanding the human emotional response to a virus is another thing altogether. HIV, COVID and now monkeypox infections all too often bring judgment and blame from some people and there is often an unseemly and unscientific search for a “patient zero” to blame. Steven Thrasher writes in The Atlantic ([link removed]) , “Journalistic and scientific writing about people living with viruses often has a dehumanizing quality.” He argues that “focusing on a virus’s origins encourages individualized shame while ignoring the broader societal factors that contribute to a disease’s transmission…stigmatizing individuals who get sick—and portraying the social, interconnected nature of communicabl
e disease as an individual matter—actually impedes efforts to slow the spread of infection.” Thrasher concludes, “We all share the responsibility of life on a planet with viruses. But those of us living without the most lethal types of them must shoulder the responsibility more. The media heap a tremendous weight on people living with disease, whether it be COVID, AIDS, or monkeypox, making them feel like they’re a burden or some kind of individual failure—and the toll of this can be deadly.”
** If You Are in a Hurry
------------------------------------------------------------
* Read Science ([link removed]) on new research that underscores probability of multiple “zoonotic events” as the origins of the virus’s jump to humans and Science ([link removed]) on the likelihood of the Wuhan market as the epicenter.
* Read Bloomberg ([link removed]) on the lack of access to monkeypox vaccines in Africa.
* Read Reuters ([link removed]) on what may happen in the northern hemisphere winter.
* Read African Journal of AIDS Research ([link removed]) on lessons learned from HIV and COVID for the next pandemics.
* Read The Guardian ([link removed]) on a study that estimates prolonged change in taste and smell among millions of people after COVID infection.
* Read STAT ([link removed]) on “Paxlovid rebound” and check out a Kaiser Health News Q&A ([link removed]) on Paxlovid.
* Read Axios ([link removed]) on a disturbing survey that found one in five Americans thought it was acceptable to threaten or harass public health officials about COVID restrictions.
** Search for the Virus Origins
------------------------------------------------------------
The authors of a research article in Science ([link removed]) (US) concluded their “findings indicate that it is unlikely that SARS-CoV-2 circulated widely in humans prior to November 2019 and define the narrow window between when SARS-CoV-2 first jumped into humans and when the first cases of COVID-19 were reported. As with other coronaviruses, SARS-CoV-2 emergence likely resulted from multiple zoonotic events.”
Another research article in Science ([link removed]) (US) concludes, “While there is insufficient evidence to define upstream events, and exact circumstances remain obscure, our analyses indicate that the emergence of SARS-CoV-2 occurred via the live wildlife trade in China, and show that the Huanan market was the epicenter of the COVID-19 pandemic.”
AP ([link removed]) (US) quotes Kristian Andersen a professor in the Department of Immunology and Microbiology at Scripps Research and coauthor of one of the studies. “All this evidence tells us the same thing: It points right to this particular market in the middle of Wuhan. I was quite convinced of the lab leak myself until we dove into this very carefully and looked at it much closer.”
** What’s Next with the Pandemic?
------------------------------------------------------------
Reuters ([link removed]) (UK) reports, “As the third winter of the coronavirus pandemic looms in the northern hemisphere, scientists are warning weary governments and populations alike to brace for more waves of COVID-19. In the United States alone, there could be up to a million infections a day this winter…. However, while cases may surge again in the coming months, deaths and hospitalizations are unlikely to rise with the same intensity, the experts said, helped by vaccination and booster drives, previous infection, milder variants and the availability of highly effective COVID treatments.”
** Lessons from COVID and HIV for the Future
------------------------------------------------------------
In a special issue of African Journal of AIDS Research ([link removed]) (South Africa) Charles Birungi, Warren Parker & Alan Whiteside argue, “It is not farfetched to assert that we seem to have entered an era of pandemics. Future pandemics will emerge more often, spread more rapidly, do more damage to the world economy, and kill more people than HIV and COVID-19, unless there is change in the global approach to dealing with infectious diseases. Without ending inequalities that drive and sustain HIV, COVID-19 and other unfinished pandemics, the world is in danger. It does not have to be this way. We can turn the tide. Indeed, the response to HIV offers many lessons.”
In the same issue ([link removed]) , Petronell Kruger and Safura Abdool Karim look at “South Africa’s regulatory response to COVID-19 through the lens of international and regional human rights law standards for pandemic control. It draws comparisons with the approach taken by the State (sometimes as mandated by South African courts) to curb the impact of HIV and AIDS in South Africa and to draw lessons for future pandemic preparedness. Our focus is on compelled public health interventions where competing human rights concerns are often stark.” They conclude: “Promoting a human rights-based approach to pandemics is mandatory under international law, but it also serves to promote the efficacy of public health responses. This is illustrated by examining South Africa’s COVID-19 response: The State failed to implement a pandemic response that accords with [international laws]; more broadly, it also departed from the human
rights-based approach it eventually adopted towards HIV. The lessons learnt from HIV and the approach adopted therein ought to be followed in the next phases of the COVID-19 response. If steps to correct the pandemic response are taken, South Africa’s response will be brought in line with its international human rights obligations and its Constitution, the spread and impact of COVID-19 will be curbed, stigma will be reduced, and trust in public health will be rebuilt.”
** EU to Buy New Spanish Vaccine
------------------------------------------------------------
AFP ([link removed]) (France) reports, “The European Commission has signed a contract to allow EU member states to buy up to 250 million doses of a new COVID-19 vaccine developed in Spain [if the vaccine is approved]…. The HIPRA vaccine, also known as PHH-1V, is protein-based and intended as a booster shot for adults whose immunity is receding after their first two or three shots.”
** What is Paxlovid Rebound?
------------------------------------------------------------
The news that US President Joe Biden has tested positive again for COVID after taking the drug paxlovid has brought “COVID rebound” into the news. STAT ([link removed]) (US) reports, “Such rebound cases following treatment with Pfizer’s five-day oral antiviral have stumped physicians as they’ve tried to understand how frequently it’s occurring and what’s allowing the virus to come back a second time…. Rebound cases have raised such questions as whether Paxlovid should be prescribed for longer courses and for which patients it should be recommended.” Read Kaiser Health News ([link removed]) Q&A ([link removed]) on Paxlovid.
** Threats to Health Officials
------------------------------------------------------------
Axios ([link removed]) (US) reports, “One in five Americans thought it was acceptable to threaten or harass public health officials over pandemic business closures as of last summer, research in JAMA Open Network ([link removed]) shows….The antagonism extended beyond science-doubters and people hurting from the effects of COVID-19, to higher earners, political independents and those with more education. A JAMA ([link removed]) (US) commentary responding to the survey argues, “Social science research affirms that no one silver bullet will reduce the hostility of political discourse at the moment, whether about politics in general nor public health in particular. However, the price of inaction and hopelessness is too high. The evidence provided by [this survey] should activate all readers to consider the many ways
in which they can advocate for more investment in public health, including advocacy for investment in the training and education of future public health professionals, supporting increased resource allocation to protect the safety and mental health of the current workforce, and individual acts of outreach to support and thank public health workers in our communities—all of which could better protect those workers on whom our collective health and well-being depend.”
** China Outbreak Stabilizes
------------------------------------------------------------
Bloomberg ([link removed]) (US) reports, “China’s latest COVID-19 outbreak has stabilized, with cases in Shanghai holding at zero for the second day in a row and the flareup in Shenzhen seemingly under control…. China’s adherence to the COVID Zero strategy, which requires mass testing, snap lockdowns and travel restrictions, has exacted a heavy economic and social toll…. President Xi Jinping has made zero tolerance for COVID a hallmark of his rule, saying the country won’t pursue ‘herd immunity’ like other nations because it would exact too much of a toll, particularly on China’s elderly, who have lower vaccination rates.”
** Long COVID
------------------------------------------------------------
The Guardian ([link removed]) (UK) reports, “Millions of people worldwide may have long-term smell or taste problems as a result of COVID-19, with women more likely to be affected, a study suggests. About 5 percent of adults infected with the coronavirus may develop long-lasting changes to their sense of smell or taste, according to the research published in the BMJ. With more than 550m confirmed COVID-19 cases to date, it means there may be long-term smell deficiencies for 15 million people and taste problems for 12 million (with an unknown overlap of those suffering both) for at least six months after an infection.” Read the BMJ ([link removed]) (UK) study.
** How Long is COVID Infectious?
------------------------------------------------------------
Nature ([link removed]) (UK) reports, “Although the question is simple — for how long is someone with COVID-19 contagious? — experts caution that the answer is complicated. ‘We always think of it as a black-and-white thing…if somebody’s infectious or not infectious — but in reality, it’s a numbers game and a probability,’ says Benjamin Meyer, a virologist at the University of Geneva in Switzerland. And that numbers game has shifting rules and baselines. Emerging variants, vaccination and varying levels of natural immunity elicited by previous infection can all influence how quickly someone can clear the virus from their system, Meyer says, and this ultimately dictates when they stop being infectious. Behavioural factors matter as well. People who feel unwell tend to mix less with others, he adds, so the severity of someone’s symptoms can influence how likely they are to infect others.”
** Monkeypox Updates
------------------------------------------------------------
NPR’s Goats and Soda blog ([link removed]) (US) reports on Dr. Dimie Ogoina, a Nigerian doctor who in 2017 diagnosed “the first case of monkeypox in Nigeria in 38 years” and watched an increase in cases in the country over the coming years, especially among young urban men. “Over the past few years, Ogoina says he has tried to warn health officials and scientists repeatedly that monkeypox had changed and was possibly spreading through sexual contact. At one international meeting, he tried to bring up the possibility of sexual transmission. Somebody told him to be quiet.” As the outbreak spread in the US and Europe, vaccination programs have been put in place, but “How many Nigerians have received the monkeypox vaccine? Zero.”
Bloomberg ([link removed]) (US) reports, “Africa, the only continent where monkeypox is endemic, has yet to receive vaccines for the virus as the infectious disease spreads around the world, the continent’s top health body said. While monkeypox was declared a public-health emergency of international concern by the head of the World Health Organization at the weekend, the Africa Centres for Disease Control and Prevention has yet to secure any doses of the inoculations… The Africa CDC is in talks with developers to get shots “as soon as possible” for both monkeypox and smallpox, Ouma said. Vaccines for the latter disease, which has been eradicated, can also be used against monkeypox. Still, Africa is dealing with at least six significant disease outbreaks aside from COVID-19 and monkeypox, including the Marburg virus, Lassa fever, cholera, measles and wild polio, putting strain on often limited
resources.”
In a statement, GAVI ([link removed]) says, “At a time when supply of this vaccine is limited, we call on countries with access to supply to share with countries that have a need for vaccines and do not have access. As the clinical data for protection against monkeypox using approved smallpox/monkeypox vaccines in the context of an outbreak of monkeypox is limited, it is critical to collect and share data on efficacy and safety in real-world settings as this vaccine is rolled out in a limited fashion to fight the outbreak.”
In a twitter thread ([link removed]) about a panel discussion at AIDS2022 Gregg Gonsalves sounds an alarm that he says conference organizers weren’t willing to sound: “With millions dead from AIDS, from COVID, thousands now infected with monkeypox, you think that we might one day treat infectious diseases as an existential threat, but we're never really able to close the deal, we just let them fester, flourish each and every darn time. To continue the fire alarm analogy—we bring a few buckets to a house fire and pat ourselves on the back, say we cannot do more or gesture to the ‘if we had political will’ or the ever present ‘we have the tools’, while people, well, just continue to suffer.”
Got this from a friend? Subscribe here. ([link removed])
============================================================
Our mailing address is:
** [email protected] (mailto:[email protected])
** unsubscribe from this list ([link removed])
** update subscription preferences ([link removed])
Message Analysis
- Sender: AVAC: Global Advocacy for HIV Prevention
- Political Party: n/a
- Country: n/a
- State/Locality: n/a
- Office: n/a
-
Email Providers:
- MailChimp
