| From | AVAC <[email protected]> |
| Subject | COVID News Brief: The news you need to know |
| Date | June 22, 2022 9:06 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
View this email in your browser ([link removed])
AVAC's weekly COVID News Brief provides a curated perspective on what COVID news is worth your time.
"In the future, we have to have enough vaccine-production capability around the world. So whenever we get a pathogen we can make so many doses so fast that this issue of who gets it first, who gets it second, becomes a non-issue. Before this pandemic, there wasn’t really a single good vaccine-manufacturing site on the continent of Africa. We’re beginning to make some changes there, but that needs to change faster. It’s also a reminder that it’s not just about having enough vaccines or therapeutics. It’s about figuring out how to help countries deploy them."
— US COVID Czar Ashish Jha in The New Yorker ([link removed])
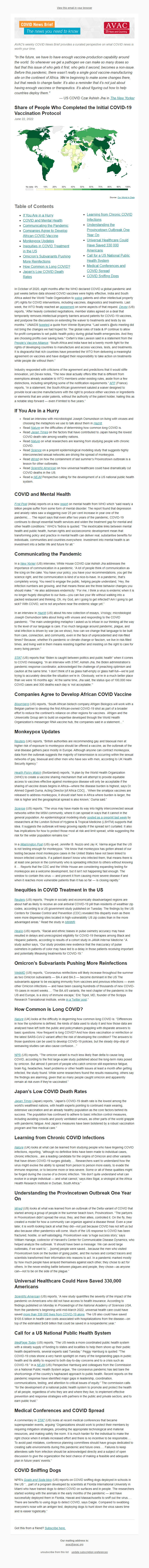
** Share of People Who Completed the Initial COVID-19 Vaccination Protocol
------------------------------------------------------------
June 22, 2022
Source: Our World in Data ([link removed])
** Table of Contents
------------------------------------------------------------
* If You Are in a Hurry (#hurry)
* COVID and Mental Health (#mental)
* Communicating the Pandemic (#comm)
* Companies Agree to Develop African COVID Vaccine (#companies)
* Monkeypox Updates (#pox)
* Inequities in COVID Treatment in the US (#inequities)
* Omicron’s Subvariants Pushing More Reinfections (#omicron)
* How Common is Long COVID? (#how)
* Japan’s Low COVID Death Rates (#japan)
* Learning from Chronic COVID Infections (#learn)
* Understanding the Provincetown Outbreak One Year On (#under)
* Universal Healthcare Could Have Saved 330,000 Americans (#universal)
* Call for a US National Public Health System (#call)
* Medical Conferences and COVID Spread (#med)
* COVID Sniffing Dogs (#sniff)
In October of 2020, eight months after the WHO declared COVID a global pandemic and just weeks before data showed COVID vaccines were highly effective, India and South Africa asked the World Trade Organization to waive ([link removed]) patents and other intellectual property (IP) rights for COVID interventions, including vaccines, diagnostics and treatments. Last week, the WTO finally reached an agreement ([link removed]) on some aspects of that request. Devex ([link removed]) (US) reports, “After heavily contested negotiations, member states agreed on a deal that temporarily removes intellectual property barriers around patents for COVID-19 vaccines, and postpone the discussions on extending the waiver to treatments and tests by six months.” UNAIDS tweeted
([link removed]) a quote from Winnie Byanyima: "Last week’s @wto meeting did not bring the changes we had hoped for. The global rules of trade & IP continue to allow for-profit companies to set public health policy during global health emergencies. And they are choosing profits over saving lives." Oxfam’s Max Lawson said in a statement from the People’s Vaccine Alliance ([link removed]) : “South Africa and India have led a twenty month fight for the rights of developing countries to manufacture and access vaccines, tests, and treatments. It is disgraceful that rich countries have prevented the WTO from delivering a meaningful agreement on vaccines and have dodged their responsibility to take action on treatments while people die without them.”
Industry responded with criticisms of the agreement and predictions that it would stifle innovation, yet Devex notes, “The new deal actually offers little that is different from exemptions already available to WTO members under existing rules, aside from a few distinctions, including simplifying some of the notification requirements.” AFP ([link removed]) (France) reports, “In a statement, the South African government saluted a waiver designed to provide local vaccine manufacturers with the right to produce either vaccines or ingredients or elements that are under patents, without the authority of the patent holder, hailing this as a notable step forward — even if limited to five years.”
** If You Are in a Hurry
------------------------------------------------------------
* Read an interview with microbiologist Joseph Osmundson on living with viruses and choosing the metaphors we use to talk about them in Hazlitt ([link removed]) .
* Read Nature ([link removed]) on the difficulties of determining how common long COVID is.
* Read Japan Times ([link removed]) on the factors that have contributed to Japan having the lowest COVID death rate among wealthy nations.
* Read Nature ([link removed]) on what researchers are learning from studying people with chronic COVID.
* Read Science ([link removed]) on a preprint epidemiological modeling study that suggests highly interconnected sexual networks are driving the spread of monkeypox.
* Read Wired ([link removed]) on how the containment of last summer’s Provincetown outbreak is a lesson for other outbreaks.
* Read Scientific American ([link removed]) on how universal healthcare could have dramatically cut COVID deaths in the US.
* Read a NEJM ([link removed]) Perspective calling for the development of a US national public health system.
** COVID and Mental Health
------------------------------------------------------------
First Post ([link removed]) (India) reports on a new report ([link removed]) on mental health from WHO which “said nearly a billion people suffer from some form of mental disorder. The report found that depression and anxiety rates saw a staggering over 25 per cent increase in year one of the pandemic…. The report says that even after two years of the pandemic, COVID-19 continues to disrupt essential health services and widen the treatment gap for mental and other health conditions.” WHO’s Tedros is quoted: “The inextricable links between mental health and public health, human rights and socioeconomic development mean that transforming policy and practice in mental health can deliver real, substantive benefits for individuals, communities and countries everywhere. Investment into mental health is an investment into a better
life and future for all.”
** Communicating the Pandemic
------------------------------------------------------------
In a New Yorker ([link removed]) (US) interview, White House COVID czar Ashish Jha addresses the importance of communication in a pandemic. “A lot of people think of communication as the icing on the cake. You have your policy, you have your recommendations, you get the science right, and the communication is kind of a nice-to-have. In a pandemic, that’s completely wrong. You need to engage the public, helping people understand, ‘Hey, the infection numbers are growing, and that means these are the three behavior changes you should make.’” He also addresses endemicity: “For me, I think a virus is endemic when it is no longer hugely disruptive to our lives—you can live your life without walking into a packed restaurant and thinking, Oh, my God, am I going to get infected? Am I going to get sick? With COVID, we’re not anywhere near the endemic stage yet.”
In an interview in Hazlitt ([link removed]) (US) about his new collection of essays, Virology, microbiologist Joseph Osmundson talks about living with viruses and responding to the COVID pandemic. “The main undergirding metaphor I asked us to infuse in our thinking all the way to the level of our language is care. If so much language around pandemic, plague, and viral infection is driven by war (as we show), how can we change that language to be built from care, connection, and community, even in the face of unprecedented and risk-filled times? Because, whether it’s pandemic or climate change or fascism, we live in risk-filled times, and living well in them means resisting together and insisting on the right to care for every living person.”
STAT ([link removed]) (US) reports that “Biden is caught between politics and public health” when it comes to COVID messaging. “In an interview with STAT, Ashish Jha, the Biden administration’s pandemic response coordinator, acknowledged the challenge of preaching optimism and caution at the same time. ‘I don’t think of it as glass half-empty or glass half-full—we’re just trying to accurately describe the situation we’re in. Obviously, we’re in a much better place than we were 16 months ago.’ At the same time, Jha said, the status quo of 100,000 new COVID cases and 300 deaths each day is ‘not acceptable.’”
** Companies Agree to Develop African COVID Vaccine
------------------------------------------------------------
Bloomberg ([link removed]) (US) reports, “South African biotech company Afrigen Biologics will work with a Belgian partner to develop the first African-owned COVID-19 shot as part of a broader effort to reduce the continent’s reliance on other regions for vaccines. Afrigen and the Univercells Group aim to build on expertise developed through the World Health Organization’s messenger RNA vaccine hub, the companies said in a statement…”
** Monkeypox Updates
------------------------------------------------------------
Reuters ([link removed]) (UK) reports, “British authorities are recommending gay and bisexual men at higher risk of exposure to monkeypox should be offered a vaccine, as the outbreak of the viral disease gathers pace mostly in Europe. Although anyone can contract monkeypox, data from the outbreak suggests the majority of transmission is occurring within the sexual networks of gay, bisexual and other men who have sex with men, according to UK Health Security Agency.”
Health Policy Watch ([link removed]) (Switzerland) reports, “A plan by the World Health Organization (WHO) to create a vaccine sharing mechanism that will attempt to provide equitable access to vaccines effective against monkeypox disease will only be acceptable if the sharing of vaccine doses begins in Africa—where the disease burden is highest, says Dr. Ahmed Ogwell Ouma, Acting Director [of Africa CDC]…‘When the smallpox vaccines are released to address monkeypox, it should start here in Africa where burden is larger, the risk is higher and the geographical spread is also known,’ Ouma said.”
Science ([link removed]) (US) reports, “The virus may have made its way into highly interconnected sexual networks within the MSM community, where it can spread in ways that it cannot in the general population. An epidemiological modeling study posted as a preprint last week ([link removed]) by researchers at the London School of Hygiene & Tropical Medicine (LSHTM) supports that idea. It suggests the outbreak will keep growing rapidly if the spread isn’t curtailed. It also has implications for how to protect those most at risk and limit spread, while suggesting the risk for the wider population remains low.”
In a Washington Post ([link removed]) (US) op-ed, Jennifer B. Nuzzo and Jay K. Varma argue that the US is not testing enough for monkeypox. “We know that monkeypox has gotten ahead of our testing because most monkeypox cases in the United States have not been linked to known infected contacts. If a patient doesn’t know who infected them, that means there is at least one person in the community who is spreading infection to others without knowing it…. Reports that the CDC and the White House are considering expanding testing for monkeypox are a welcome development, but it isn’t not happening fast enough. The window to contain this virus — and prevent it from causing more severe disease if and when it reaches more vulnerable patients than it has so far — is closing rapidly.”
** Inequities in COVID Treatment in the US
------------------------------------------------------------
Reuters ([link removed]) (US) reports, “People in socially and economically disadvantaged regions are about half as likely to receive an oral antiviral COVID-19 pill than residents of wealthier zip codes, according to a US government study published on Tuesday. The findings by the US Centers for Disease Control and Prevention (CDC) revealed this disparity even as there were more dispensing sites located in high-vulnerability US zip codes than in the more advantaged areas.” Read the study in MMWR ([link removed]) .
Healio ([link removed]) (US) reports, “Racial and ethnic biases in pulse oximetry accuracy may have resulted in delays and unrecognized eligibility for COVID-19 therapies among Black and Hispanic patients, according to results of a cohort study in JAMA Internal Medicine.” A study author says, “Our study provides new evidence that the inaccuracy of pulse oximeters in patients of color may have led to a delay in those patients receiving important and potentially lifesaving treatments for COVID-19.”
** Omicron’s Subvariants Pushing More Reinfections
------------------------------------------------------------
WebMD ([link removed]) (US) reports, “Coronavirus reinfections will likely increase throughout the summer as two Omicron subvariants — BA.4 and BA.5 — become dominant in the US The subvariants appear to be escaping immunity from vaccines and previous infections — even other Omicron infections — and have been causing hundreds of thousands of new COVID-19 cases in recent weeks…. ‘The BA.4/5 variants, the next chapter of the pandemic in the US and Europe, is a story of immune escape,’ Eric Topol, MD, founder of the Scripps Research Translational Institute, wrote in a Twitter post ([link removed]) .”
** How Common is Long COVID?
------------------------------------------------------------
Nature ([link removed]) (UK) looks at the difficulty in degerming how common long COVID is: “Differences in how the syndrome is defined, the kinds of data used to study it and how those data are analysed have left both the public and policymakers grappling with disparate answers to basic questions. How frequent is long COVID? And how does vaccination or reinfection or the latest SARS-CoV-2 variant affect the risk of developing the condition? The answers to those questions can be used to develop COVID-19 policies, but the steady drip–drip of seesawing studies can also cause confusion…”
NPR ([link removed]) (US) reports, “The omicron variant is much less likely than delta to cause long COVID, according to the first large-scale study published about the long-term risks posed by omicron. But almost 5 percent of people who catch omicron still experience fatigue, brain fog, headaches, heart problems or other health issues at least a month after getting infected, the study found. While some researchers found the results reassuring, others say the findings are alarming, given that so many people caught omicron and apparently remain at risk even if they're vaccinated.”
** Japan’s Low COVID Death Rates
------------------------------------------------------------
Japan Times ([link removed]) (Japan) reports, “Japan’s COVID-19 death rate is the lowest among the world’s wealthiest nations, with health experts pointing to continued mask wearing, extensive vaccination and an already healthy population as the core factors behind its success. The population has continued to adhere to basic infection control measures, including avoiding crowds and poorly ventilated venues, as other parts of the world grapple with pandemic fatigue. And Japan’s measures have been bolstered by a robust vaccination program and free medical care.”
** Learning from Chronic COVID Infections
------------------------------------------------------------
Nature ([link removed]) (UK) looks at what can be learned from studying people who have lingering COVID infections, reporting, “although no definitive links have been made to individual cases, chronic infections…are a leading candidate for the origins of Omicron and other variants that have driven COVID-19 surges globally…. Researchers want to understand how the virus might evolve the ability to spread from person to person more easily, to evade the immune response, or to become more or less severe. Some or all of these qualities might be forged during the course of a chronic infection. ‘We don’t quite understand what can evolve in a single individual — and what cannot,’ says Alex Sigal, a virologist at the Africa Health Research Institute in Durban, South Africa.”
** Understanding the Provincetown Outbreak One Year On
------------------------------------------------------------
Wired ([link removed]) (US) looks at what was learned from an outbreak of the Delta variant of COVID that started among a group of people in the summer beach town, Provincetown. “The partyers in Provincetown didn’t spread the virus; they, and their allies, controlled it. On the fly, they created a model for how a community can organize against a disease threat. Even a year later, it is worth looking back at what they did—not just because COVID has not left us but also because other pandemics will come. Much of the US response to COVID has been fractured, hostile, or self-sabotaging. Provincetown was ‘a huge success story,’ says William Hanage, codirector of Harvard’s Center for Communicable Disease Dynamics, who helped analyze the outbreak. ‘It should have been a message: We can avoid large outbreaks, if we want to.’…[some] people were saved…because the men who visited Provincetown took on the burden of going public, and the nurses
and contact tracers and scientists transformed their information into reasons to act. In a pandemic marked mostly by how much people have arrayed themselves against each other, they chose to act for others. In the never-ending battle between plagues and people, they chose—as anyone can—not to be on the side of the plague.”
** Universal Healthcare Could Have Saved 330,000 Americans
------------------------------------------------------------
Scientific American ([link removed]) (US) reports, “A new study quantifies the severity of the impact of the pandemic on Americans who did not have access to health insurance. According to findings published on Monday in Proceedings of the National Academy of Sciences USA, from the pandemic’s beginning until mid-March 2022, universal health care could have saved more than 338,000 lives from COVID-19 alone ([link removed]) . The US also could have saved $105.6 billion in health care costs associated with hospitalizations from the disease—on top of the estimated $438 billion that could be saved in a nonpandemic year.”
** Call for a US National Public Health System
------------------------------------------------------------
MedPage Today ([link removed]) (US) reports, “The US needs a more coordinated public health system with a steady supply of funding to states and localities to help them shore up their public health departments, several experts said Tuesday.” Peggy Hamburg is quoted: "The COVID-19 crisis shone a very harsh spotlight on many of the longstanding gaps in public health and its ability to respond to both day-to-day concerns and to a crisis such as COVID-19.” In a NEJM ([link removed]) (US) Perspective Hamburg and colleagues from the Commission on a National Public Health System argue, “the coronavirus pandemic has laid bare the shortcomings of the country’s haphazard approach to public health. Recent reports on the pandemic response have identified major gaps in leadership, coordination, communications, testing, and attention to critical issues of equity.” The commission calls “for the development of a
national public health system to promote and protect the health of all people, regardless of who they are and where they live; to implement effective prevention and response strategies with partners in the public and private sectors; and to earn public trust.”
** Medical Conferences and COVID Spread
------------------------------------------------------------
A commentary in STAT ([link removed]) (US) looks at recent medical conferences that became superspreader events, arguing “Organizations should work to protect their members by requiring mitigation strategies, providing the appropriate technological and material resources, and making safety the norm. It is much harder for the individual to make the right choice when it entails increased effort and there is no incentive to be responsible…. To avoid past mistakes, conference planning committees should have groups dedicated to creating safe environments during this pandemic and future ones…. Failures to keep attendees safe from infection should be acknowledged directly and a subject of open discussion to give the organization the best chance of making a feasible and adequate plan in future years’ events.”
** COVID Sniffing Dogs
------------------------------------------------------------
NPR’s Goats and Soda blog ([link removed]) (US) reports on COVID sniffing dogs deployed in schools in the US “…part of a program developed by scientists at Florida International University in Miami who have trained dogs to detect COVID on surfaces and in people. The researchers started working with the animals in the early months of the pandemic — and have successfully deployed them in Florida, Hawaii and Massachusetts to sniff out the virus…. There are benefits to using dogs to detect COVID, says Daigle. Compared to swabbing everyone's nose with an antigen test, deploying dogs to hunt down the virus saves time and is easier logistically.”
Got this from a friend? Subscribe here. ([link removed])
============================================================
Our mailing address is:
** [email protected] (mailto:[email protected])
** unsubscribe from this list ([link removed])
** update subscription preferences ([link removed])
AVAC's weekly COVID News Brief provides a curated perspective on what COVID news is worth your time.
"In the future, we have to have enough vaccine-production capability around the world. So whenever we get a pathogen we can make so many doses so fast that this issue of who gets it first, who gets it second, becomes a non-issue. Before this pandemic, there wasn’t really a single good vaccine-manufacturing site on the continent of Africa. We’re beginning to make some changes there, but that needs to change faster. It’s also a reminder that it’s not just about having enough vaccines or therapeutics. It’s about figuring out how to help countries deploy them."
— US COVID Czar Ashish Jha in The New Yorker ([link removed])
** Share of People Who Completed the Initial COVID-19 Vaccination Protocol
------------------------------------------------------------
June 22, 2022
Source: Our World in Data ([link removed])
** Table of Contents
------------------------------------------------------------
* If You Are in a Hurry (#hurry)
* COVID and Mental Health (#mental)
* Communicating the Pandemic (#comm)
* Companies Agree to Develop African COVID Vaccine (#companies)
* Monkeypox Updates (#pox)
* Inequities in COVID Treatment in the US (#inequities)
* Omicron’s Subvariants Pushing More Reinfections (#omicron)
* How Common is Long COVID? (#how)
* Japan’s Low COVID Death Rates (#japan)
* Learning from Chronic COVID Infections (#learn)
* Understanding the Provincetown Outbreak One Year On (#under)
* Universal Healthcare Could Have Saved 330,000 Americans (#universal)
* Call for a US National Public Health System (#call)
* Medical Conferences and COVID Spread (#med)
* COVID Sniffing Dogs (#sniff)
In October of 2020, eight months after the WHO declared COVID a global pandemic and just weeks before data showed COVID vaccines were highly effective, India and South Africa asked the World Trade Organization to waive ([link removed]) patents and other intellectual property (IP) rights for COVID interventions, including vaccines, diagnostics and treatments. Last week, the WTO finally reached an agreement ([link removed]) on some aspects of that request. Devex ([link removed]) (US) reports, “After heavily contested negotiations, member states agreed on a deal that temporarily removes intellectual property barriers around patents for COVID-19 vaccines, and postpone the discussions on extending the waiver to treatments and tests by six months.” UNAIDS tweeted
([link removed]) a quote from Winnie Byanyima: "Last week’s @wto meeting did not bring the changes we had hoped for. The global rules of trade & IP continue to allow for-profit companies to set public health policy during global health emergencies. And they are choosing profits over saving lives." Oxfam’s Max Lawson said in a statement from the People’s Vaccine Alliance ([link removed]) : “South Africa and India have led a twenty month fight for the rights of developing countries to manufacture and access vaccines, tests, and treatments. It is disgraceful that rich countries have prevented the WTO from delivering a meaningful agreement on vaccines and have dodged their responsibility to take action on treatments while people die without them.”
Industry responded with criticisms of the agreement and predictions that it would stifle innovation, yet Devex notes, “The new deal actually offers little that is different from exemptions already available to WTO members under existing rules, aside from a few distinctions, including simplifying some of the notification requirements.” AFP ([link removed]) (France) reports, “In a statement, the South African government saluted a waiver designed to provide local vaccine manufacturers with the right to produce either vaccines or ingredients or elements that are under patents, without the authority of the patent holder, hailing this as a notable step forward — even if limited to five years.”
** If You Are in a Hurry
------------------------------------------------------------
* Read an interview with microbiologist Joseph Osmundson on living with viruses and choosing the metaphors we use to talk about them in Hazlitt ([link removed]) .
* Read Nature ([link removed]) on the difficulties of determining how common long COVID is.
* Read Japan Times ([link removed]) on the factors that have contributed to Japan having the lowest COVID death rate among wealthy nations.
* Read Nature ([link removed]) on what researchers are learning from studying people with chronic COVID.
* Read Science ([link removed]) on a preprint epidemiological modeling study that suggests highly interconnected sexual networks are driving the spread of monkeypox.
* Read Wired ([link removed]) on how the containment of last summer’s Provincetown outbreak is a lesson for other outbreaks.
* Read Scientific American ([link removed]) on how universal healthcare could have dramatically cut COVID deaths in the US.
* Read a NEJM ([link removed]) Perspective calling for the development of a US national public health system.
** COVID and Mental Health
------------------------------------------------------------
First Post ([link removed]) (India) reports on a new report ([link removed]) on mental health from WHO which “said nearly a billion people suffer from some form of mental disorder. The report found that depression and anxiety rates saw a staggering over 25 per cent increase in year one of the pandemic…. The report says that even after two years of the pandemic, COVID-19 continues to disrupt essential health services and widen the treatment gap for mental and other health conditions.” WHO’s Tedros is quoted: “The inextricable links between mental health and public health, human rights and socioeconomic development mean that transforming policy and practice in mental health can deliver real, substantive benefits for individuals, communities and countries everywhere. Investment into mental health is an investment into a better
life and future for all.”
** Communicating the Pandemic
------------------------------------------------------------
In a New Yorker ([link removed]) (US) interview, White House COVID czar Ashish Jha addresses the importance of communication in a pandemic. “A lot of people think of communication as the icing on the cake. You have your policy, you have your recommendations, you get the science right, and the communication is kind of a nice-to-have. In a pandemic, that’s completely wrong. You need to engage the public, helping people understand, ‘Hey, the infection numbers are growing, and that means these are the three behavior changes you should make.’” He also addresses endemicity: “For me, I think a virus is endemic when it is no longer hugely disruptive to our lives—you can live your life without walking into a packed restaurant and thinking, Oh, my God, am I going to get infected? Am I going to get sick? With COVID, we’re not anywhere near the endemic stage yet.”
In an interview in Hazlitt ([link removed]) (US) about his new collection of essays, Virology, microbiologist Joseph Osmundson talks about living with viruses and responding to the COVID pandemic. “The main undergirding metaphor I asked us to infuse in our thinking all the way to the level of our language is care. If so much language around pandemic, plague, and viral infection is driven by war (as we show), how can we change that language to be built from care, connection, and community, even in the face of unprecedented and risk-filled times? Because, whether it’s pandemic or climate change or fascism, we live in risk-filled times, and living well in them means resisting together and insisting on the right to care for every living person.”
STAT ([link removed]) (US) reports that “Biden is caught between politics and public health” when it comes to COVID messaging. “In an interview with STAT, Ashish Jha, the Biden administration’s pandemic response coordinator, acknowledged the challenge of preaching optimism and caution at the same time. ‘I don’t think of it as glass half-empty or glass half-full—we’re just trying to accurately describe the situation we’re in. Obviously, we’re in a much better place than we were 16 months ago.’ At the same time, Jha said, the status quo of 100,000 new COVID cases and 300 deaths each day is ‘not acceptable.’”
** Companies Agree to Develop African COVID Vaccine
------------------------------------------------------------
Bloomberg ([link removed]) (US) reports, “South African biotech company Afrigen Biologics will work with a Belgian partner to develop the first African-owned COVID-19 shot as part of a broader effort to reduce the continent’s reliance on other regions for vaccines. Afrigen and the Univercells Group aim to build on expertise developed through the World Health Organization’s messenger RNA vaccine hub, the companies said in a statement…”
** Monkeypox Updates
------------------------------------------------------------
Reuters ([link removed]) (UK) reports, “British authorities are recommending gay and bisexual men at higher risk of exposure to monkeypox should be offered a vaccine, as the outbreak of the viral disease gathers pace mostly in Europe. Although anyone can contract monkeypox, data from the outbreak suggests the majority of transmission is occurring within the sexual networks of gay, bisexual and other men who have sex with men, according to UK Health Security Agency.”
Health Policy Watch ([link removed]) (Switzerland) reports, “A plan by the World Health Organization (WHO) to create a vaccine sharing mechanism that will attempt to provide equitable access to vaccines effective against monkeypox disease will only be acceptable if the sharing of vaccine doses begins in Africa—where the disease burden is highest, says Dr. Ahmed Ogwell Ouma, Acting Director [of Africa CDC]…‘When the smallpox vaccines are released to address monkeypox, it should start here in Africa where burden is larger, the risk is higher and the geographical spread is also known,’ Ouma said.”
Science ([link removed]) (US) reports, “The virus may have made its way into highly interconnected sexual networks within the MSM community, where it can spread in ways that it cannot in the general population. An epidemiological modeling study posted as a preprint last week ([link removed]) by researchers at the London School of Hygiene & Tropical Medicine (LSHTM) supports that idea. It suggests the outbreak will keep growing rapidly if the spread isn’t curtailed. It also has implications for how to protect those most at risk and limit spread, while suggesting the risk for the wider population remains low.”
In a Washington Post ([link removed]) (US) op-ed, Jennifer B. Nuzzo and Jay K. Varma argue that the US is not testing enough for monkeypox. “We know that monkeypox has gotten ahead of our testing because most monkeypox cases in the United States have not been linked to known infected contacts. If a patient doesn’t know who infected them, that means there is at least one person in the community who is spreading infection to others without knowing it…. Reports that the CDC and the White House are considering expanding testing for monkeypox are a welcome development, but it isn’t not happening fast enough. The window to contain this virus — and prevent it from causing more severe disease if and when it reaches more vulnerable patients than it has so far — is closing rapidly.”
** Inequities in COVID Treatment in the US
------------------------------------------------------------
Reuters ([link removed]) (US) reports, “People in socially and economically disadvantaged regions are about half as likely to receive an oral antiviral COVID-19 pill than residents of wealthier zip codes, according to a US government study published on Tuesday. The findings by the US Centers for Disease Control and Prevention (CDC) revealed this disparity even as there were more dispensing sites located in high-vulnerability US zip codes than in the more advantaged areas.” Read the study in MMWR ([link removed]) .
Healio ([link removed]) (US) reports, “Racial and ethnic biases in pulse oximetry accuracy may have resulted in delays and unrecognized eligibility for COVID-19 therapies among Black and Hispanic patients, according to results of a cohort study in JAMA Internal Medicine.” A study author says, “Our study provides new evidence that the inaccuracy of pulse oximeters in patients of color may have led to a delay in those patients receiving important and potentially lifesaving treatments for COVID-19.”
** Omicron’s Subvariants Pushing More Reinfections
------------------------------------------------------------
WebMD ([link removed]) (US) reports, “Coronavirus reinfections will likely increase throughout the summer as two Omicron subvariants — BA.4 and BA.5 — become dominant in the US The subvariants appear to be escaping immunity from vaccines and previous infections — even other Omicron infections — and have been causing hundreds of thousands of new COVID-19 cases in recent weeks…. ‘The BA.4/5 variants, the next chapter of the pandemic in the US and Europe, is a story of immune escape,’ Eric Topol, MD, founder of the Scripps Research Translational Institute, wrote in a Twitter post ([link removed]) .”
** How Common is Long COVID?
------------------------------------------------------------
Nature ([link removed]) (UK) looks at the difficulty in degerming how common long COVID is: “Differences in how the syndrome is defined, the kinds of data used to study it and how those data are analysed have left both the public and policymakers grappling with disparate answers to basic questions. How frequent is long COVID? And how does vaccination or reinfection or the latest SARS-CoV-2 variant affect the risk of developing the condition? The answers to those questions can be used to develop COVID-19 policies, but the steady drip–drip of seesawing studies can also cause confusion…”
NPR ([link removed]) (US) reports, “The omicron variant is much less likely than delta to cause long COVID, according to the first large-scale study published about the long-term risks posed by omicron. But almost 5 percent of people who catch omicron still experience fatigue, brain fog, headaches, heart problems or other health issues at least a month after getting infected, the study found. While some researchers found the results reassuring, others say the findings are alarming, given that so many people caught omicron and apparently remain at risk even if they're vaccinated.”
** Japan’s Low COVID Death Rates
------------------------------------------------------------
Japan Times ([link removed]) (Japan) reports, “Japan’s COVID-19 death rate is the lowest among the world’s wealthiest nations, with health experts pointing to continued mask wearing, extensive vaccination and an already healthy population as the core factors behind its success. The population has continued to adhere to basic infection control measures, including avoiding crowds and poorly ventilated venues, as other parts of the world grapple with pandemic fatigue. And Japan’s measures have been bolstered by a robust vaccination program and free medical care.”
** Learning from Chronic COVID Infections
------------------------------------------------------------
Nature ([link removed]) (UK) looks at what can be learned from studying people who have lingering COVID infections, reporting, “although no definitive links have been made to individual cases, chronic infections…are a leading candidate for the origins of Omicron and other variants that have driven COVID-19 surges globally…. Researchers want to understand how the virus might evolve the ability to spread from person to person more easily, to evade the immune response, or to become more or less severe. Some or all of these qualities might be forged during the course of a chronic infection. ‘We don’t quite understand what can evolve in a single individual — and what cannot,’ says Alex Sigal, a virologist at the Africa Health Research Institute in Durban, South Africa.”
** Understanding the Provincetown Outbreak One Year On
------------------------------------------------------------
Wired ([link removed]) (US) looks at what was learned from an outbreak of the Delta variant of COVID that started among a group of people in the summer beach town, Provincetown. “The partyers in Provincetown didn’t spread the virus; they, and their allies, controlled it. On the fly, they created a model for how a community can organize against a disease threat. Even a year later, it is worth looking back at what they did—not just because COVID has not left us but also because other pandemics will come. Much of the US response to COVID has been fractured, hostile, or self-sabotaging. Provincetown was ‘a huge success story,’ says William Hanage, codirector of Harvard’s Center for Communicable Disease Dynamics, who helped analyze the outbreak. ‘It should have been a message: We can avoid large outbreaks, if we want to.’…[some] people were saved…because the men who visited Provincetown took on the burden of going public, and the nurses
and contact tracers and scientists transformed their information into reasons to act. In a pandemic marked mostly by how much people have arrayed themselves against each other, they chose to act for others. In the never-ending battle between plagues and people, they chose—as anyone can—not to be on the side of the plague.”
** Universal Healthcare Could Have Saved 330,000 Americans
------------------------------------------------------------
Scientific American ([link removed]) (US) reports, “A new study quantifies the severity of the impact of the pandemic on Americans who did not have access to health insurance. According to findings published on Monday in Proceedings of the National Academy of Sciences USA, from the pandemic’s beginning until mid-March 2022, universal health care could have saved more than 338,000 lives from COVID-19 alone ([link removed]) . The US also could have saved $105.6 billion in health care costs associated with hospitalizations from the disease—on top of the estimated $438 billion that could be saved in a nonpandemic year.”
** Call for a US National Public Health System
------------------------------------------------------------
MedPage Today ([link removed]) (US) reports, “The US needs a more coordinated public health system with a steady supply of funding to states and localities to help them shore up their public health departments, several experts said Tuesday.” Peggy Hamburg is quoted: "The COVID-19 crisis shone a very harsh spotlight on many of the longstanding gaps in public health and its ability to respond to both day-to-day concerns and to a crisis such as COVID-19.” In a NEJM ([link removed]) (US) Perspective Hamburg and colleagues from the Commission on a National Public Health System argue, “the coronavirus pandemic has laid bare the shortcomings of the country’s haphazard approach to public health. Recent reports on the pandemic response have identified major gaps in leadership, coordination, communications, testing, and attention to critical issues of equity.” The commission calls “for the development of a
national public health system to promote and protect the health of all people, regardless of who they are and where they live; to implement effective prevention and response strategies with partners in the public and private sectors; and to earn public trust.”
** Medical Conferences and COVID Spread
------------------------------------------------------------
A commentary in STAT ([link removed]) (US) looks at recent medical conferences that became superspreader events, arguing “Organizations should work to protect their members by requiring mitigation strategies, providing the appropriate technological and material resources, and making safety the norm. It is much harder for the individual to make the right choice when it entails increased effort and there is no incentive to be responsible…. To avoid past mistakes, conference planning committees should have groups dedicated to creating safe environments during this pandemic and future ones…. Failures to keep attendees safe from infection should be acknowledged directly and a subject of open discussion to give the organization the best chance of making a feasible and adequate plan in future years’ events.”
** COVID Sniffing Dogs
------------------------------------------------------------
NPR’s Goats and Soda blog ([link removed]) (US) reports on COVID sniffing dogs deployed in schools in the US “…part of a program developed by scientists at Florida International University in Miami who have trained dogs to detect COVID on surfaces and in people. The researchers started working with the animals in the early months of the pandemic — and have successfully deployed them in Florida, Hawaii and Massachusetts to sniff out the virus…. There are benefits to using dogs to detect COVID, says Daigle. Compared to swabbing everyone's nose with an antigen test, deploying dogs to hunt down the virus saves time and is easier logistically.”
Got this from a friend? Subscribe here. ([link removed])
============================================================
Our mailing address is:
** [email protected] (mailto:[email protected])
** unsubscribe from this list ([link removed])
** update subscription preferences ([link removed])
Message Analysis
- Sender: AVAC: Global Advocacy for HIV Prevention
- Political Party: n/a
- Country: n/a
- State/Locality: n/a
- Office: n/a
-
Email Providers:
- MailChimp
