| From | ADEA <[email protected]> |
| Subject | ADEA Advocate - July 20, 2021 |
| Date | July 21, 2021 2:08 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
View this email in your browser [ [link removed] ] .
American Dental Education Association
Volume 2, No. 19, July 20, 2021
ADEA Advocacy in Action
This appears weekly in the ADEA Advocate to summarize and provide direct links to recent advocacy actions taken by ADEA. Please let us know what you think and how we might improve its usefulness.
Issues and Resources
• Provider Relief Fund Reporting portal [ [link removed] ]
• ADEA memo [ [link removed] ] regarding vaccines at the state level
• ADEA report [ [link removed] ] on the Impact of the COVID-19 Pandemic on U.S. Dental Schools
• ADEA policy brief [ [link removed] ] regarding overprescription of antibiotics
• For a full list of ADEA memos, briefs and letters click here [ [link removed] ] .
Medicaid Expansion Update
In Missouri [ [link removed] ] , the debate over Medicaid expansion has reached the state’s Supreme Court. In August 2020, voters in the state passed a ballot measure that added to the state’s constitution a requirement to implement the expansion. During the following legislative session, however, the Missouri General Assembly refused to provide funding for the expansion and, as a result, Gov. Mike Parson (R) dropped plans for expanding the program [ [link removed] ] . The decision to drop the program was quickly challenged in the state’s court system, and a lower court sided with the state [ [link removed] ] in June, ruling that the ballot measure was unconstitutional because it attempted to spend state funds without identifying a funding source. The state’s Supreme Court began its review of the ruling on July 13.
In contrast, Oklahoma [ [link removed] ] implemented their state expansion on July 1. Like Missouri, voters in Oklahoma also passed a ballot initiative in 2020 requiring the state to implement the expansion. State officials estimate that nearly 200,000 people are eligible for Medicaid under the expansion and have reported that more than 133,000 have been approved for benefits.
Meanwhile, Democrats in Congress are debating [ [link removed] ] several plans to close the Medicaid gap in the states that have not yet implemented expansion. The proposed plans include allowing local governments to implement expansion, requiring the federal government to offer a Medicaid-like plan in holdout states and offering financial incentives to encourage states to adopt expansion on their own.
Dental Education Programs Fare Well in FY 2022 HHS Budget
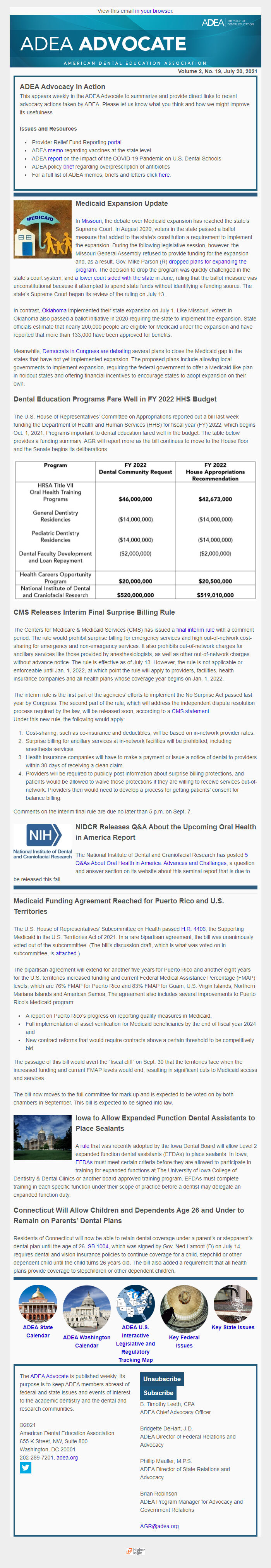
The U.S. House of Representatives’ Committee on Appropriations reported out a bill last week funding the Department of Health and Human Services (HHS) for fiscal year (FY) 2022, which begins Oct. 1, 2021. Programs important to dental education fared well in the budget. The table below provides a funding summary. AGR will report more as the bill continues to move to the House floor and the Senate begins its deliberations.
CMS Releases Interim Final Surprise Billing Rule
The Centers for Medicare & Medicaid Services (CMS) has issued a final interim rule [ [link removed] ] with a comment period. The rule would prohibit surprise billing for emergency services and high out-of-network cost-sharing for emergency and non-emergency services. It also prohibits out-of-network charges for ancillary services like those provided by anesthesiologists, as well as other out-of-network charges without advance notice. The rule is effective as of July 13. However, the rule is not applicable or enforceable until Jan. 1, 2022, at which point the rule will apply to providers, facilities, health insurance companies and all health plans whose coverage year begins on Jan. 1, 2022.
The interim rule is the first part of the agencies’ efforts to implement the No Surprise Act passed last year by Congress. The second part of the rule, which will address the independent dispute resolution process required by the law, will be released soon, according to a CMS statement [ [link removed] ] .
Under this new rule, the following would apply:
1. Cost-sharing, such as co-insurance and deductibles, will be based on in-network provider rates.
2. Surprise billing for ancillary services at in-network facilities will be prohibited, including anesthesia services.
3. Health insurance companies will have to make a payment or issue a notice of denial to providers within 30 days of receiving a clean claim.
4. Providers will be required to publicly post information about surprise-billing protections, and patients would be allowed to waive those protections if they are willing to receive services out-of-network. Providers then would need to develop a process for getting patients’ consent for balance billing.
Comments on the interim final rule are due no later than 5 p.m. on Sept. 7.
NIDCR Releases Q&A About the Upcoming Oral Health in America Report
The National Institute of Dental and Craniofacial Research has posted 5 Q&As About Oral Health in America: Advances and Challenges [ [link removed] ] , a question and answer section on its website about this seminal report that is due to be released this fall.
Medicaid Funding Agreement Reached for Puerto Rico and U.S. Territories
The U.S. House of Representatives’ Subcommittee on Health passed H.R. 4406 [ [link removed] ] , the Supporting Medicaid in the U.S. Territories Act of 2021. In a rare bipartisan agreement, the bill was unanimously voted out of the subcommittee. (The bill’s discussion draft, which is what was voted on in subcommittee, is attached [ [link removed] ] .)
The bipartisan agreement will extend for another five years for Puerto Rico and another eight years for the U.S. territories increased funding and current Federal Medical Assistance Percentage (FMAP) levels, which are 76% FMAP for Puerto Rico and 83% FMAP for Guam, U.S. Virgin Islands, Northern Mariana Islands and American Samoa. The agreement also includes several improvements to Puerto Rico’s Medicaid program:
• A report on Puerto Rico’s progress on reporting quality measures in Medicaid,
• Full implementation of asset verification for Medicaid beneficiaries by the end of fiscal year 2024 and
• New contract reforms that would require contracts above a certain threshold to be competitively bid.
The passage of this bill would avert the “fiscal cliff” on Sept. 30 that the territories face when the increased funding and current FMAP levels would end, resulting in significant cuts to Medicaid access and services.
The bill now moves to the full committee for mark up and is expected to be voted on by both chambers in September. This bill is expected to be signed into law.
Iowa to Allow Expanded Function Dental Assistants to Place Sealants
A rule [ [link removed] ] that was recently adopted by the Iowa Dental Board will allow Level 2 expanded function dental assistants (EFDAs) to place sealants. In Iowa, EFDAs [ [link removed] ] must meet certain criteria before they are allowed to participate in training for expanded functions at The University of Iowa College of Dentistry & Dental Clinics or another board-approved training program. EFDAs must complete training in each specific function under their scope of practice before a dentist may delegate an expanded function duty.
Connecticut Will Allow Children and Dependents Age 26 and Under to Remain on Parents’ Dental Plans
Residents of Connecticut will now be able to retain dental coverage under a parent's or stepparent’s dental plan until the age of 26. SB 1004 [ [link removed] ] , which was signed by Gov. Ned Lamont (D) on July 14, requires dental and vision insurance policies to continue coverage for a child, stepchild or other dependent child until the child turns 26 years old. The bill also added a requirement that all health plans provide coverage to stepchildren or other dependent children.
ADEA State Calendar [ [link removed] ]
ADEA Washington Calendar [ [link removed] ]
ADEA U.S. Interactive Legislative and Regulatory Tracking Map [ [link removed] ]
Key Federal Issues [ [link removed] ]
Key State Issues [ [link removed] ]
The ADEA Advocate [ [link removed] ] is published weekly. Its purpose is to keep ADEA members abreast of federal and state issues and events of interest to the academic dentistry and the dental and research communities.
©2021
American Dental Education Association
655 K Street, NW, Suite 800
Washington, DC 20001
202-289-7201, adea.org [ [link removed] ]
twitter
[link removed]
Unsubscribe
[link removed]
Subscribe
[link removed][0]&p_colname=p_last_nm&p_varname=p_val_arr[1]&p_colname=p_alias&p_varname=p_val_arr[2]&p_colname=p_login_id&p_varname=p_val_arr[3]&p_colname=p_passwd&p_context=NEWSLETTER&p_success_url=censsaindprofile.section_update%3Fp_profile_ty%3DINDIVIDUAL_PROFILE%26p_skip_confirm_fl%3DY%26p_section_nm%3DNewsletters%26p_format%3D110%26p_msg_txt%3D%26p_cust_id%3D%26p_referrer%3Dadeacenssalandingpage.display_page%3Fp_context%3DNEWSLETTER
B. Timothy Leeth, CPA
ADEA Chief Advocacy Officer
Bridgette DeHart, J.D.
ADEA Director of Federal Relations and Advocacy
Phillip Mauller, M.P.S.
ADEA Director of State Relations and Advocacy
Brian Robinson
ADEA Program Manager for Advocacy and Government Relations
[email protected] [ [link removed] ]
Powered by Higher Logic [link removed]
American Dental Education Association
Volume 2, No. 19, July 20, 2021
ADEA Advocacy in Action
This appears weekly in the ADEA Advocate to summarize and provide direct links to recent advocacy actions taken by ADEA. Please let us know what you think and how we might improve its usefulness.
Issues and Resources
• Provider Relief Fund Reporting portal [ [link removed] ]
• ADEA memo [ [link removed] ] regarding vaccines at the state level
• ADEA report [ [link removed] ] on the Impact of the COVID-19 Pandemic on U.S. Dental Schools
• ADEA policy brief [ [link removed] ] regarding overprescription of antibiotics
• For a full list of ADEA memos, briefs and letters click here [ [link removed] ] .
Medicaid Expansion Update
In Missouri [ [link removed] ] , the debate over Medicaid expansion has reached the state’s Supreme Court. In August 2020, voters in the state passed a ballot measure that added to the state’s constitution a requirement to implement the expansion. During the following legislative session, however, the Missouri General Assembly refused to provide funding for the expansion and, as a result, Gov. Mike Parson (R) dropped plans for expanding the program [ [link removed] ] . The decision to drop the program was quickly challenged in the state’s court system, and a lower court sided with the state [ [link removed] ] in June, ruling that the ballot measure was unconstitutional because it attempted to spend state funds without identifying a funding source. The state’s Supreme Court began its review of the ruling on July 13.
In contrast, Oklahoma [ [link removed] ] implemented their state expansion on July 1. Like Missouri, voters in Oklahoma also passed a ballot initiative in 2020 requiring the state to implement the expansion. State officials estimate that nearly 200,000 people are eligible for Medicaid under the expansion and have reported that more than 133,000 have been approved for benefits.
Meanwhile, Democrats in Congress are debating [ [link removed] ] several plans to close the Medicaid gap in the states that have not yet implemented expansion. The proposed plans include allowing local governments to implement expansion, requiring the federal government to offer a Medicaid-like plan in holdout states and offering financial incentives to encourage states to adopt expansion on their own.
Dental Education Programs Fare Well in FY 2022 HHS Budget
The U.S. House of Representatives’ Committee on Appropriations reported out a bill last week funding the Department of Health and Human Services (HHS) for fiscal year (FY) 2022, which begins Oct. 1, 2021. Programs important to dental education fared well in the budget. The table below provides a funding summary. AGR will report more as the bill continues to move to the House floor and the Senate begins its deliberations.
CMS Releases Interim Final Surprise Billing Rule
The Centers for Medicare & Medicaid Services (CMS) has issued a final interim rule [ [link removed] ] with a comment period. The rule would prohibit surprise billing for emergency services and high out-of-network cost-sharing for emergency and non-emergency services. It also prohibits out-of-network charges for ancillary services like those provided by anesthesiologists, as well as other out-of-network charges without advance notice. The rule is effective as of July 13. However, the rule is not applicable or enforceable until Jan. 1, 2022, at which point the rule will apply to providers, facilities, health insurance companies and all health plans whose coverage year begins on Jan. 1, 2022.
The interim rule is the first part of the agencies’ efforts to implement the No Surprise Act passed last year by Congress. The second part of the rule, which will address the independent dispute resolution process required by the law, will be released soon, according to a CMS statement [ [link removed] ] .
Under this new rule, the following would apply:
1. Cost-sharing, such as co-insurance and deductibles, will be based on in-network provider rates.
2. Surprise billing for ancillary services at in-network facilities will be prohibited, including anesthesia services.
3. Health insurance companies will have to make a payment or issue a notice of denial to providers within 30 days of receiving a clean claim.
4. Providers will be required to publicly post information about surprise-billing protections, and patients would be allowed to waive those protections if they are willing to receive services out-of-network. Providers then would need to develop a process for getting patients’ consent for balance billing.
Comments on the interim final rule are due no later than 5 p.m. on Sept. 7.
NIDCR Releases Q&A About the Upcoming Oral Health in America Report
The National Institute of Dental and Craniofacial Research has posted 5 Q&As About Oral Health in America: Advances and Challenges [ [link removed] ] , a question and answer section on its website about this seminal report that is due to be released this fall.
Medicaid Funding Agreement Reached for Puerto Rico and U.S. Territories
The U.S. House of Representatives’ Subcommittee on Health passed H.R. 4406 [ [link removed] ] , the Supporting Medicaid in the U.S. Territories Act of 2021. In a rare bipartisan agreement, the bill was unanimously voted out of the subcommittee. (The bill’s discussion draft, which is what was voted on in subcommittee, is attached [ [link removed] ] .)
The bipartisan agreement will extend for another five years for Puerto Rico and another eight years for the U.S. territories increased funding and current Federal Medical Assistance Percentage (FMAP) levels, which are 76% FMAP for Puerto Rico and 83% FMAP for Guam, U.S. Virgin Islands, Northern Mariana Islands and American Samoa. The agreement also includes several improvements to Puerto Rico’s Medicaid program:
• A report on Puerto Rico’s progress on reporting quality measures in Medicaid,
• Full implementation of asset verification for Medicaid beneficiaries by the end of fiscal year 2024 and
• New contract reforms that would require contracts above a certain threshold to be competitively bid.
The passage of this bill would avert the “fiscal cliff” on Sept. 30 that the territories face when the increased funding and current FMAP levels would end, resulting in significant cuts to Medicaid access and services.
The bill now moves to the full committee for mark up and is expected to be voted on by both chambers in September. This bill is expected to be signed into law.
Iowa to Allow Expanded Function Dental Assistants to Place Sealants
A rule [ [link removed] ] that was recently adopted by the Iowa Dental Board will allow Level 2 expanded function dental assistants (EFDAs) to place sealants. In Iowa, EFDAs [ [link removed] ] must meet certain criteria before they are allowed to participate in training for expanded functions at The University of Iowa College of Dentistry & Dental Clinics or another board-approved training program. EFDAs must complete training in each specific function under their scope of practice before a dentist may delegate an expanded function duty.
Connecticut Will Allow Children and Dependents Age 26 and Under to Remain on Parents’ Dental Plans
Residents of Connecticut will now be able to retain dental coverage under a parent's or stepparent’s dental plan until the age of 26. SB 1004 [ [link removed] ] , which was signed by Gov. Ned Lamont (D) on July 14, requires dental and vision insurance policies to continue coverage for a child, stepchild or other dependent child until the child turns 26 years old. The bill also added a requirement that all health plans provide coverage to stepchildren or other dependent children.
ADEA State Calendar [ [link removed] ]
ADEA Washington Calendar [ [link removed] ]
ADEA U.S. Interactive Legislative and Regulatory Tracking Map [ [link removed] ]
Key Federal Issues [ [link removed] ]
Key State Issues [ [link removed] ]
The ADEA Advocate [ [link removed] ] is published weekly. Its purpose is to keep ADEA members abreast of federal and state issues and events of interest to the academic dentistry and the dental and research communities.
©2021
American Dental Education Association
655 K Street, NW, Suite 800
Washington, DC 20001
202-289-7201, adea.org [ [link removed] ]
[link removed]
Unsubscribe
[link removed]
Subscribe
[link removed][0]&p_colname=p_last_nm&p_varname=p_val_arr[1]&p_colname=p_alias&p_varname=p_val_arr[2]&p_colname=p_login_id&p_varname=p_val_arr[3]&p_colname=p_passwd&p_context=NEWSLETTER&p_success_url=censsaindprofile.section_update%3Fp_profile_ty%3DINDIVIDUAL_PROFILE%26p_skip_confirm_fl%3DY%26p_section_nm%3DNewsletters%26p_format%3D110%26p_msg_txt%3D%26p_cust_id%3D%26p_referrer%3Dadeacenssalandingpage.display_page%3Fp_context%3DNEWSLETTER
B. Timothy Leeth, CPA
ADEA Chief Advocacy Officer
Bridgette DeHart, J.D.
ADEA Director of Federal Relations and Advocacy
Phillip Mauller, M.P.S.
ADEA Director of State Relations and Advocacy
Brian Robinson
ADEA Program Manager for Advocacy and Government Relations
[email protected] [ [link removed] ]
Powered by Higher Logic [link removed]
Message Analysis
- Sender: American Dental Education Association (ADEA)
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
