Email
North Carolina’s Health Agency Is Failing — With Full Pockets
| From | NC Political Tea <[email protected]> |
| Subject | North Carolina’s Health Agency Is Failing — With Full Pockets |
| Date | January 20, 2026 3:49 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
View this post on the web at [link removed]
North Carolina’s Department of Health and Human Services (DHHS) oversees everything from food assistance and Medicaid to long-term care. But according to multiple audits, the agency is falling short on its core mission — despite having the money to do better.
The most striking number: $386 million in unspent salary funds [ [link removed] ] in a single fiscal year. That funding had been approved to hire staff in critical roles — intake workers, Medicaid processors, nursing home inspectors. Instead, the money lapsed. DHHS, which is legally required to file reports on those lapses, has submitted them an average of 296 days late since 2017.
$386 million unspent. $83 million in delayed food aid. 700,000 new Medicaid enrollees. All inside one state agency.
I took a hard look at North Carolina’s Department of Health and Human Services — and what I found was alarming.
Despite record funding and growing public need, DHHS has repeatedly failed to deliver basic services on time. Delayed SNAP benefits, under-regulated nursing homes, and Medicaid payments to suspended providers are just the start.
A February 2025 audit revealed that DHHS continued to reimburse Medicaid providers with suspended or restricted licenses, even after they had been flagged for serious violations — including fraud, neglect, and improper care delivery.
$386 million unspent. $83 million in delayed food aid. 700,000 new Medicaid enrollees. All inside one state agency.
Unfit Providers: Patients at Risk While Tax Dollars Flowed
Last July, the State Auditor released its annual report [ [link removed] ] on DHHS’ Medicaid Provider program— and the findings were alarming. The audit shows that some of the most serious failures were not technical errors but decisions that left Medicaid patients in harm’s way while unfit providers continued to be paid with public funds.
In one of the most alarming cases, a physician who was explicitly barred from treating female patients due to prior sexual and professional misconduct remained enrolled in Medicaid. Despite the restriction, the provider continued seeing patients, including 21 women, and Medicaid paid more than $7,300 in 2023 alone. The same physician had previously agreed to repay $75,000 for fraudulent Medicaid billing, yet no documented risk assessment or removal followed.
The audit also found that providers who were legally prohibited from practicing at all—continued treating Medicaid patients and billing the state.
One physician treated patients while restricted for alcohol abuse; another continued practicing for months after being barred for improperly prescribing controlled substances to friends and romantic partners. In both cases, Medicaid paid for care that should never have been provided.
Finally, the state failed to verify DEA certification, allowing providers without required authorization to prescribe controlled substances. Auditors identified multiple cases in which uncertified providers wrote prescriptions that were filled, even as Medicaid paid tens of thousands of dollars for their services.
One such provider later pleaded guilty to federal drug crimes.
Taken together, these cases show a clear pattern: known risks were ignored, enforcement was weakened, and patients were exposed to dangerous providers while taxpayer money continued to flow.
In Nursing Homes, A Complaint—and Then Silence
Long-term care facilities are supposed to be closely monitored. But according to North Carolina Health News [ [link removed] ], complaints about neglect and unsafe conditions often vanish into a black hole.
One woman reported mold and bruises at her mother’s nursing home. Eight months later, she got a reply.
DHHS blamed “staffing shortages.” But that’s hard to square with the hundreds of millions left unspent on staffing.
State records show the agency had 1,300 vacancies in critical oversight and clinical roles during the same reporting period.
Medicaid Spending Soars — But Where’s the Care?
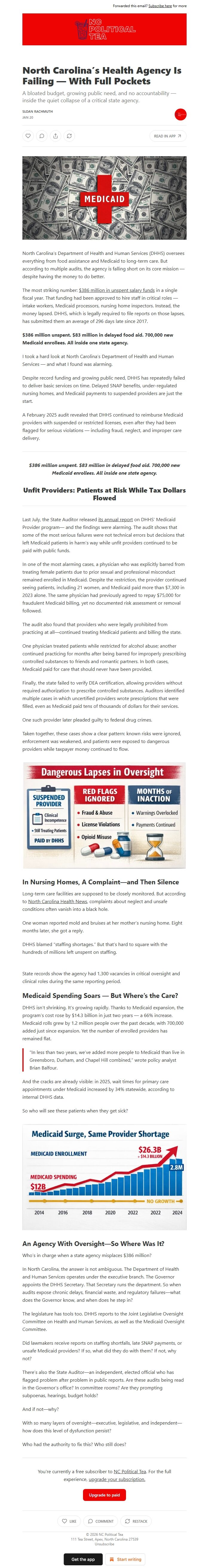
DHHS isn’t shrinking. It’s growing rapidly. Thanks to Medicaid expansion, the program’s cost rose by $14.3 billion in just two years — a 66% increase. Medicaid rolls grew by 1.2 million people over the past decade, with 700,000 added just since expansion. Yet the number of enrolled providers has remained flat.
“In less than two years, we’ve added more people to Medicaid than live in Greensboro, Durham, and Chapel Hill combined,” wrote policy analyst Brian Balfour.
And the cracks are already visible: in 2025, wait times for primary care appointments under Medicaid increased by 34% statewide, according to internal DHHS data.
So who will see these patients when they get sick?
An Agency With Oversight—So Where Was It?
Who’s in charge when a state agency misplaces $386 million?
In North Carolina, the answer is not ambiguous. The Department of Health and Human Services operates under the executive branch. The Governor appoints the DHHS Secretary. That Secretary runs the department. So when audits expose chronic delays, financial waste, and regulatory failures—what does the Governor know, and when does he step in?
The legislature has tools too. DHHS reports to the Joint Legislative Oversight Committee on Health and Human Services, as well as the Medicaid Oversight Committee.
Did lawmakers receive reports on staffing shortfalls, late SNAP payments, or unsafe Medicaid providers? If so, what did they do with them? If not, why not?
There’s also the State Auditor—an independent, elected official who has flagged problem after problem in public reports. Are these audits being read in the Governor’s office? In committee rooms? Are they prompting subpoenas, hearings, budget holds?
And if not—why?
With so many layers of oversight—executive, legislative, and independent—how does this level of dysfunction persist?
Who had the authority to fix this? Who still does?
Unsubscribe [link removed]?
North Carolina’s Department of Health and Human Services (DHHS) oversees everything from food assistance and Medicaid to long-term care. But according to multiple audits, the agency is falling short on its core mission — despite having the money to do better.
The most striking number: $386 million in unspent salary funds [ [link removed] ] in a single fiscal year. That funding had been approved to hire staff in critical roles — intake workers, Medicaid processors, nursing home inspectors. Instead, the money lapsed. DHHS, which is legally required to file reports on those lapses, has submitted them an average of 296 days late since 2017.
$386 million unspent. $83 million in delayed food aid. 700,000 new Medicaid enrollees. All inside one state agency.
I took a hard look at North Carolina’s Department of Health and Human Services — and what I found was alarming.
Despite record funding and growing public need, DHHS has repeatedly failed to deliver basic services on time. Delayed SNAP benefits, under-regulated nursing homes, and Medicaid payments to suspended providers are just the start.
A February 2025 audit revealed that DHHS continued to reimburse Medicaid providers with suspended or restricted licenses, even after they had been flagged for serious violations — including fraud, neglect, and improper care delivery.
$386 million unspent. $83 million in delayed food aid. 700,000 new Medicaid enrollees. All inside one state agency.
Unfit Providers: Patients at Risk While Tax Dollars Flowed
Last July, the State Auditor released its annual report [ [link removed] ] on DHHS’ Medicaid Provider program— and the findings were alarming. The audit shows that some of the most serious failures were not technical errors but decisions that left Medicaid patients in harm’s way while unfit providers continued to be paid with public funds.
In one of the most alarming cases, a physician who was explicitly barred from treating female patients due to prior sexual and professional misconduct remained enrolled in Medicaid. Despite the restriction, the provider continued seeing patients, including 21 women, and Medicaid paid more than $7,300 in 2023 alone. The same physician had previously agreed to repay $75,000 for fraudulent Medicaid billing, yet no documented risk assessment or removal followed.
The audit also found that providers who were legally prohibited from practicing at all—continued treating Medicaid patients and billing the state.
One physician treated patients while restricted for alcohol abuse; another continued practicing for months after being barred for improperly prescribing controlled substances to friends and romantic partners. In both cases, Medicaid paid for care that should never have been provided.
Finally, the state failed to verify DEA certification, allowing providers without required authorization to prescribe controlled substances. Auditors identified multiple cases in which uncertified providers wrote prescriptions that were filled, even as Medicaid paid tens of thousands of dollars for their services.
One such provider later pleaded guilty to federal drug crimes.
Taken together, these cases show a clear pattern: known risks were ignored, enforcement was weakened, and patients were exposed to dangerous providers while taxpayer money continued to flow.
In Nursing Homes, A Complaint—and Then Silence
Long-term care facilities are supposed to be closely monitored. But according to North Carolina Health News [ [link removed] ], complaints about neglect and unsafe conditions often vanish into a black hole.
One woman reported mold and bruises at her mother’s nursing home. Eight months later, she got a reply.
DHHS blamed “staffing shortages.” But that’s hard to square with the hundreds of millions left unspent on staffing.
State records show the agency had 1,300 vacancies in critical oversight and clinical roles during the same reporting period.
Medicaid Spending Soars — But Where’s the Care?
DHHS isn’t shrinking. It’s growing rapidly. Thanks to Medicaid expansion, the program’s cost rose by $14.3 billion in just two years — a 66% increase. Medicaid rolls grew by 1.2 million people over the past decade, with 700,000 added just since expansion. Yet the number of enrolled providers has remained flat.
“In less than two years, we’ve added more people to Medicaid than live in Greensboro, Durham, and Chapel Hill combined,” wrote policy analyst Brian Balfour.
And the cracks are already visible: in 2025, wait times for primary care appointments under Medicaid increased by 34% statewide, according to internal DHHS data.
So who will see these patients when they get sick?
An Agency With Oversight—So Where Was It?
Who’s in charge when a state agency misplaces $386 million?
In North Carolina, the answer is not ambiguous. The Department of Health and Human Services operates under the executive branch. The Governor appoints the DHHS Secretary. That Secretary runs the department. So when audits expose chronic delays, financial waste, and regulatory failures—what does the Governor know, and when does he step in?
The legislature has tools too. DHHS reports to the Joint Legislative Oversight Committee on Health and Human Services, as well as the Medicaid Oversight Committee.
Did lawmakers receive reports on staffing shortfalls, late SNAP payments, or unsafe Medicaid providers? If so, what did they do with them? If not, why not?
There’s also the State Auditor—an independent, elected official who has flagged problem after problem in public reports. Are these audits being read in the Governor’s office? In committee rooms? Are they prompting subpoenas, hearings, budget holds?
And if not—why?
With so many layers of oversight—executive, legislative, and independent—how does this level of dysfunction persist?
Who had the authority to fix this? Who still does?
Unsubscribe [link removed]?
Message Analysis
- Sender: n/a
- Political Party: n/a
- Country: n/a
- State/Locality: n/a
- Office: n/a
