| From | xxxxxx <[email protected]> |
| Subject | The Real Fraud, Waste, and Abuse |
| Date | November 9, 2025 1:05 AM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
[[link removed]]
THE REAL FRAUD, WASTE, AND ABUSE
[[link removed]]
Adam Gaffney, Danny McCormick, Steffie Woolhandler, David Himmelstein
November 7, 2025
Health Affairs
[[link removed]]
*
[[link removed]]
*
[[link removed]]
*
*
[[link removed]]
_ Medicare And Medicaid Privatization _
,
President Donald Trump and Elon Musk’s Department of Government
Efficiency (DOGE) have taken a chainsaw to the US federal government,
slashing programs, personnel, research, and global aid. The recently
enacted One Big Beautiful Bill Act (OBBBA) budget reconciliation
package, meanwhile, cuts nearly $1 trillion from Medicaid and the
Affordable Care Act over the next decade—adding more than 10 million
[[link removed]] to the ranks of the uninsured.
The OBBBA also slashes nearly $290 billion
[[link removed]] from food subsidies for the
poor and could trigger $490 billion
[[link removed]] in cuts
from Medicare.
The president and his congressional allies claim these cuts are needed
remedies for waste, fraud, and abuse. Yet, they turn a blind eye to
the trillions of dollars that private insurers drain from the public
Medicare and Medicaid programs. Indeed, one of the administration’s
first health financing actions—augmenting payments to Medicare’s
private-insurance subcontractors—will add $25 billion
[[link removed]]
to that waste in the coming year alone. If the administration were
serious about curbing waste and inefficiency, it would start by
reducing the diversion of public funds to these corporate
intermediaries.
Medicare Advantage Overpayments
Medicaid and Medicare, established in 1965 as publicly administered
health insurance programs for the poor and elderly, respectively, have
since the 1980s increasingly subcontracted coverage to private health
insurance firms (ostensibly to improve efficiency); government pays
them premiums, and the firms pay the providers. For decades, the
Medicare Payment Advisory Commission (MedPAC)—Medicare’s official
monitor—has warned that such privatization raises costs. Yet, today,
more than half
[[link removed]]
of Medicare beneficiaries are covered by private Medicare Advantage
(MA) insurers, lured by ubiquitous ads promising lower out-of-pocket
costs and extra benefits (for example, dental care and eyeglasses).
Meanwhile, state governments, which run Medicaid, now consign 75
percent
[[link removed]]
of Medicaid beneficiaries to private, mostly for-profit, managed care
plans.
MA insurers use various maneuvers (some legal and some not) to extract
overpayments (that is, payments exceeding the costs that Medicare
would have incurred had MA enrollees been covered under publicly
administered Medicare). Those maneuvers fall into two categories:
“upcoding,” that is, exaggerating enrollees’ severity of illness
to collect higher premiums from Medicare (from which, according to
MedPAC
[[link removed]],
insurers in MA garnered overpayments of $38 billion in 2024); and
favorable selection, that is, avoiding (or ejecting) unprofitably ill
enrollees, which raised taxpayers’ cost by an additional $41
billion.
Combined, upcoding plus favorable selection boosted taxpayers’ costs
for MA by more than $600 billion between 2007 and 2024; during that
period, MA plans’ overhead (a category encompassing profits as well
as expenditures for marketing, executives’ salaries, and the managed
care bureaucracy that deters care) totaled $592 billion
[[link removed]],
or 97 percent of the overpayments. For 2025, MedPAC estimates that MA
overpayments will boost taxpayers’ cost for MA enrollees by 20
percent
[[link removed]].
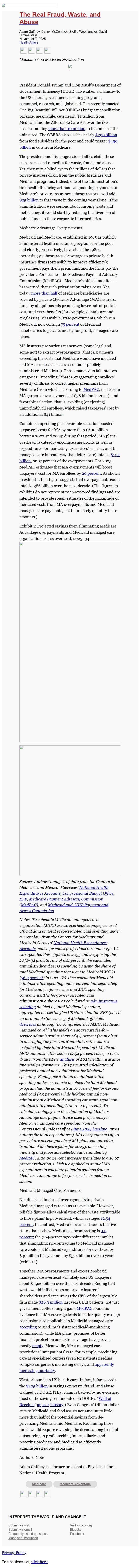
As shown in exhibit 1, that figure suggests that overpayments could
total $1,386 billion over the next decade. (The figures in exhibit 1
do not represent peer-reviewed findings and are intended to provide
rough estimates of the magnitude of increased costs from MA
overpayments and Medicaid managed care payments, not to precisely
quantify these amounts.)
Exhibit 1: Projected savings from eliminating Medicare Advantage
overpayments and Medicaid managed care organization excess overhead,
2025–34
_Source: Authors’ analysis of data from the Centers for Medicare and
Medicaid Services’ __National Health Expenditures Accounts_
[[link removed]]_,
__Congressional Budget Office_
[[link removed]]_,
__KFF_
[[link removed]]_,
__Medicare Payment Advisory Commission (MedPAC)_
[[link removed]]_,
and __Medicaid and CHIP Payment and Access Commission_
[[link removed]]_._
_Notes: To calculate Medicaid managed care organization (MCO) excess
overhead savings, we used official data on total projected Medicaid
spending under current law from the Centers for Medicare and Medicaid
Services’ __National Health Expenditures Accounts_
[[link removed]]_,
which provides projections through 2032. We extrapolated these figures
to 2033 and 2034 using the 2031–32 growth rate of 6.11 percent. We
calculated annual Medicaid MCO spending by using the share of total
Medicaid spending that went to Medicaid MCOs (__56.9 percent_
[[link removed]]_)
in 2022. We then calculated Medicaid administrative spending under
current law separately for Medicaid fee-for-service and MCO spending
components. The fee-for-service Medicaid administrative share was
calculated as __administrative spending_
[[link removed]]_
divided by total Medicaid spending, aggregated across the five US
states that the KFF (based on its annual state survey of Medicaid
officials) __describes_
[[link removed]]_
as having “no comprehensive MMC [Medicaid managed care].” This
yields an aggregate fee-for-service administrative share of 4.9
percent (equivalent to averaging the five states’ administrative
shares weighted by their total Medicaid spending). Medicaid MCO
administrative share (12.54 percent) was, in turn, drawn from the
KFF’s __analysis_
[[link removed]]_
of 2023 health insurance financial performance. This permitted
calculation of projected annual non-administrative Medicaid spending.
Finally, we estimated administrative spending under a scenario in
which the total Medicaid program had the administrative costs of
fee-for-service Medicaid (4.9 percent) while holding annual
non-administrative Medicaid spending constant, equal
non-administrative spending/(100.0–4.9 percent). To calculate
savings from the elimination of Medicare Advantage overpayments, we
used projections for Medicare managed care spending from the
Congressional Budget Office (__June 2024 baseline_
[[link removed]]_;
gross outlays for total expenditures). MA overpayments of 20 percent
are overpayments of MA plans compared to traditional Medicare plans
for 2025 from coding intensity and favorable selection as estimated by
__MedPAC_
[[link removed]]_.
A 20.00 percent increase translates to a 16.67 percent reduction,
which we applied to annual MA expenditures to calculate potential
savings from a Medicare Advantage to fee-for-service transition as
shown._
Medicaid Managed Care Payments
No official estimates of overpayments to private Medicaid managed care
plans are available. However, reliable figures allow calculation of
the waste attributable to those plans’ high overhead, which averages
12.54 percent
[[link removed]].
In contrast, Medicaid overhead across the five states that eschew
Medicaid subcontracting is 4.9 percent
[[link removed]];
the 7.64-percentage-point difference implies that eliminating
subcontracting to Medicaid managed care could cut Medicaid
expenditures for overhead by $40 billion this year and by $534 billion
over 10 years (exhibit 1).
Together, MA overpayments and excess Medicaid managed care overhead
will likely cost US taxpayers about $1,920 billion over the next
decade. Ending that waste would inflict losses on private insurers’
shareholders and executives (the CEO of the largest MA firm made $26.3
million
[[link removed]]
last year). But patients, not just government coffers, might gain.
MedPAC
[[link removed]]
found no evidence that MA coverage leads to better quality care, (a
conclusion also applicable to Medicaid managed care according
[[link removed]] to
MedPAC’s sister Medicaid-monitoring commission), while MA plans’
promises of better financial protection and extra coverage have proven
mostly empty [[link removed]].
Meanwhile, MA’s managed care restrictions limit patients’ care,
for example, precluding care at specialized centers (even for patients
needing complex surgeries), increasing delays, and apparently
increasing mortality
[[link removed]].
Waste abounds in US health care. In fact, it far exceeds the $205
billion [[link removed]] in savings on waste, fraud, and
abuse claimed by DOGE. (That claim is backed by no evidence; most of
the savings enumerated on DOGE’s “Wall of Receipts
[[link removed]]” appear
[[link removed]]
illusory
[[link removed]].)
Even Congress’ trillion-dollar cuts to Medicaid and food assistance
amount to little more than half of the potential savings from
de-privatizing Medicaid and Medicare. Reclaiming those funds would
require reversing the decades-long trend of outsourcing to
profit-seeking intermediaries and restoring Medicare and Medicaid as
efficiently administered public programs.
Authors’ Note
Adam Gaffney is a former president of Physicians for a National Health
Program.
* Medicare
[[link removed]]
* Medicare Advantage
[[link removed]]
*
[[link removed]]
*
[[link removed]]
*
*
[[link removed]]
INTERPRET THE WORLD AND CHANGE IT
Submit via web
[[link removed]]
Submit via email
Frequently asked questions
[[link removed]]
Manage subscription
[[link removed]]
Visit xxxxxx.org
[[link removed]]
Bluesky [[link removed]]
Facebook [[link removed]]
[link removed]
To unsubscribe, click the following link:
[link removed]
THE REAL FRAUD, WASTE, AND ABUSE
[[link removed]]
Adam Gaffney, Danny McCormick, Steffie Woolhandler, David Himmelstein
November 7, 2025
Health Affairs
[[link removed]]
*
[[link removed]]
*
[[link removed]]
*
*
[[link removed]]
_ Medicare And Medicaid Privatization _
,
President Donald Trump and Elon Musk’s Department of Government
Efficiency (DOGE) have taken a chainsaw to the US federal government,
slashing programs, personnel, research, and global aid. The recently
enacted One Big Beautiful Bill Act (OBBBA) budget reconciliation
package, meanwhile, cuts nearly $1 trillion from Medicaid and the
Affordable Care Act over the next decade—adding more than 10 million
[[link removed]] to the ranks of the uninsured.
The OBBBA also slashes nearly $290 billion
[[link removed]] from food subsidies for the
poor and could trigger $490 billion
[[link removed]] in cuts
from Medicare.
The president and his congressional allies claim these cuts are needed
remedies for waste, fraud, and abuse. Yet, they turn a blind eye to
the trillions of dollars that private insurers drain from the public
Medicare and Medicaid programs. Indeed, one of the administration’s
first health financing actions—augmenting payments to Medicare’s
private-insurance subcontractors—will add $25 billion
[[link removed]]
to that waste in the coming year alone. If the administration were
serious about curbing waste and inefficiency, it would start by
reducing the diversion of public funds to these corporate
intermediaries.
Medicare Advantage Overpayments
Medicaid and Medicare, established in 1965 as publicly administered
health insurance programs for the poor and elderly, respectively, have
since the 1980s increasingly subcontracted coverage to private health
insurance firms (ostensibly to improve efficiency); government pays
them premiums, and the firms pay the providers. For decades, the
Medicare Payment Advisory Commission (MedPAC)—Medicare’s official
monitor—has warned that such privatization raises costs. Yet, today,
more than half
[[link removed]]
of Medicare beneficiaries are covered by private Medicare Advantage
(MA) insurers, lured by ubiquitous ads promising lower out-of-pocket
costs and extra benefits (for example, dental care and eyeglasses).
Meanwhile, state governments, which run Medicaid, now consign 75
percent
[[link removed]]
of Medicaid beneficiaries to private, mostly for-profit, managed care
plans.
MA insurers use various maneuvers (some legal and some not) to extract
overpayments (that is, payments exceeding the costs that Medicare
would have incurred had MA enrollees been covered under publicly
administered Medicare). Those maneuvers fall into two categories:
“upcoding,” that is, exaggerating enrollees’ severity of illness
to collect higher premiums from Medicare (from which, according to
MedPAC
[[link removed]],
insurers in MA garnered overpayments of $38 billion in 2024); and
favorable selection, that is, avoiding (or ejecting) unprofitably ill
enrollees, which raised taxpayers’ cost by an additional $41
billion.
Combined, upcoding plus favorable selection boosted taxpayers’ costs
for MA by more than $600 billion between 2007 and 2024; during that
period, MA plans’ overhead (a category encompassing profits as well
as expenditures for marketing, executives’ salaries, and the managed
care bureaucracy that deters care) totaled $592 billion
[[link removed]],
or 97 percent of the overpayments. For 2025, MedPAC estimates that MA
overpayments will boost taxpayers’ cost for MA enrollees by 20
percent
[[link removed]].
As shown in exhibit 1, that figure suggests that overpayments could
total $1,386 billion over the next decade. (The figures in exhibit 1
do not represent peer-reviewed findings and are intended to provide
rough estimates of the magnitude of increased costs from MA
overpayments and Medicaid managed care payments, not to precisely
quantify these amounts.)
Exhibit 1: Projected savings from eliminating Medicare Advantage
overpayments and Medicaid managed care organization excess overhead,
2025–34
_Source: Authors’ analysis of data from the Centers for Medicare and
Medicaid Services’ __National Health Expenditures Accounts_
[[link removed]]_,
__Congressional Budget Office_
[[link removed]]_,
__KFF_
[[link removed]]_,
__Medicare Payment Advisory Commission (MedPAC)_
[[link removed]]_,
and __Medicaid and CHIP Payment and Access Commission_
[[link removed]]_._
_Notes: To calculate Medicaid managed care organization (MCO) excess
overhead savings, we used official data on total projected Medicaid
spending under current law from the Centers for Medicare and Medicaid
Services’ __National Health Expenditures Accounts_
[[link removed]]_,
which provides projections through 2032. We extrapolated these figures
to 2033 and 2034 using the 2031–32 growth rate of 6.11 percent. We
calculated annual Medicaid MCO spending by using the share of total
Medicaid spending that went to Medicaid MCOs (__56.9 percent_
[[link removed]]_)
in 2022. We then calculated Medicaid administrative spending under
current law separately for Medicaid fee-for-service and MCO spending
components. The fee-for-service Medicaid administrative share was
calculated as __administrative spending_
[[link removed]]_
divided by total Medicaid spending, aggregated across the five US
states that the KFF (based on its annual state survey of Medicaid
officials) __describes_
[[link removed]]_
as having “no comprehensive MMC [Medicaid managed care].” This
yields an aggregate fee-for-service administrative share of 4.9
percent (equivalent to averaging the five states’ administrative
shares weighted by their total Medicaid spending). Medicaid MCO
administrative share (12.54 percent) was, in turn, drawn from the
KFF’s __analysis_
[[link removed]]_
of 2023 health insurance financial performance. This permitted
calculation of projected annual non-administrative Medicaid spending.
Finally, we estimated administrative spending under a scenario in
which the total Medicaid program had the administrative costs of
fee-for-service Medicaid (4.9 percent) while holding annual
non-administrative Medicaid spending constant, equal
non-administrative spending/(100.0–4.9 percent). To calculate
savings from the elimination of Medicare Advantage overpayments, we
used projections for Medicare managed care spending from the
Congressional Budget Office (__June 2024 baseline_
[[link removed]]_;
gross outlays for total expenditures). MA overpayments of 20 percent
are overpayments of MA plans compared to traditional Medicare plans
for 2025 from coding intensity and favorable selection as estimated by
__MedPAC_
[[link removed]]_.
A 20.00 percent increase translates to a 16.67 percent reduction,
which we applied to annual MA expenditures to calculate potential
savings from a Medicare Advantage to fee-for-service transition as
shown._
Medicaid Managed Care Payments
No official estimates of overpayments to private Medicaid managed care
plans are available. However, reliable figures allow calculation of
the waste attributable to those plans’ high overhead, which averages
12.54 percent
[[link removed]].
In contrast, Medicaid overhead across the five states that eschew
Medicaid subcontracting is 4.9 percent
[[link removed]];
the 7.64-percentage-point difference implies that eliminating
subcontracting to Medicaid managed care could cut Medicaid
expenditures for overhead by $40 billion this year and by $534 billion
over 10 years (exhibit 1).
Together, MA overpayments and excess Medicaid managed care overhead
will likely cost US taxpayers about $1,920 billion over the next
decade. Ending that waste would inflict losses on private insurers’
shareholders and executives (the CEO of the largest MA firm made $26.3
million
[[link removed]]
last year). But patients, not just government coffers, might gain.
MedPAC
[[link removed]]
found no evidence that MA coverage leads to better quality care, (a
conclusion also applicable to Medicaid managed care according
[[link removed]] to
MedPAC’s sister Medicaid-monitoring commission), while MA plans’
promises of better financial protection and extra coverage have proven
mostly empty [[link removed]].
Meanwhile, MA’s managed care restrictions limit patients’ care,
for example, precluding care at specialized centers (even for patients
needing complex surgeries), increasing delays, and apparently
increasing mortality
[[link removed]].
Waste abounds in US health care. In fact, it far exceeds the $205
billion [[link removed]] in savings on waste, fraud, and
abuse claimed by DOGE. (That claim is backed by no evidence; most of
the savings enumerated on DOGE’s “Wall of Receipts
[[link removed]]” appear
[[link removed]]
illusory
[[link removed]].)
Even Congress’ trillion-dollar cuts to Medicaid and food assistance
amount to little more than half of the potential savings from
de-privatizing Medicaid and Medicare. Reclaiming those funds would
require reversing the decades-long trend of outsourcing to
profit-seeking intermediaries and restoring Medicare and Medicaid as
efficiently administered public programs.
Authors’ Note
Adam Gaffney is a former president of Physicians for a National Health
Program.
* Medicare
[[link removed]]
* Medicare Advantage
[[link removed]]
*
[[link removed]]
*
[[link removed]]
*
*
[[link removed]]
INTERPRET THE WORLD AND CHANGE IT
Submit via web
[[link removed]]
Submit via email
Frequently asked questions
[[link removed]]
Manage subscription
[[link removed]]
Visit xxxxxx.org
[[link removed]]
Bluesky [[link removed]]
Facebook [[link removed]]
[link removed]
To unsubscribe, click the following link:
[link removed]
Message Analysis
- Sender: Portside
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
