Email
EVV Impacts due to Dual Demonstration Pilot Program Discontinued effective January 1, 2026
| From | Texas Health and Human Services Commission <[email protected]> |
| Subject | EVV Impacts due to Dual Demonstration Pilot Program Discontinued effective January 1, 2026 |
| Date | September 30, 2025 2:32 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
Having trouble viewing this email? View it as a Web page [ [link removed] ].
HHS Logo [ [link removed] ]
EVV Impacts due to Dual Demonstration Pilot Program Discontinued effective January 1, 2026
Beginning January 1, 2026, HHSC will discontinue the Dual Demonstration Program with the Medicare-Medicaid Plans (MMPs) in the listed demonstration counties:
* Bexar County: Molina Healthcare of Texas.
* Dallas County: Molina Healthcare of Texas and Superior Health Plan.
* El Paso County: Molina Healthcare of Texas.
* Harris County: Molina Healthcare of Texas and United Healthcare.
* Hidalgo County: Molina Healthcare of Texas and Superior Health Plan.
HHSC will end the MMP plan codes in the demonstration counties. MMP members will choose a STAR+PLUS Managed Care Organization (MCO) in their service area to continue their services.
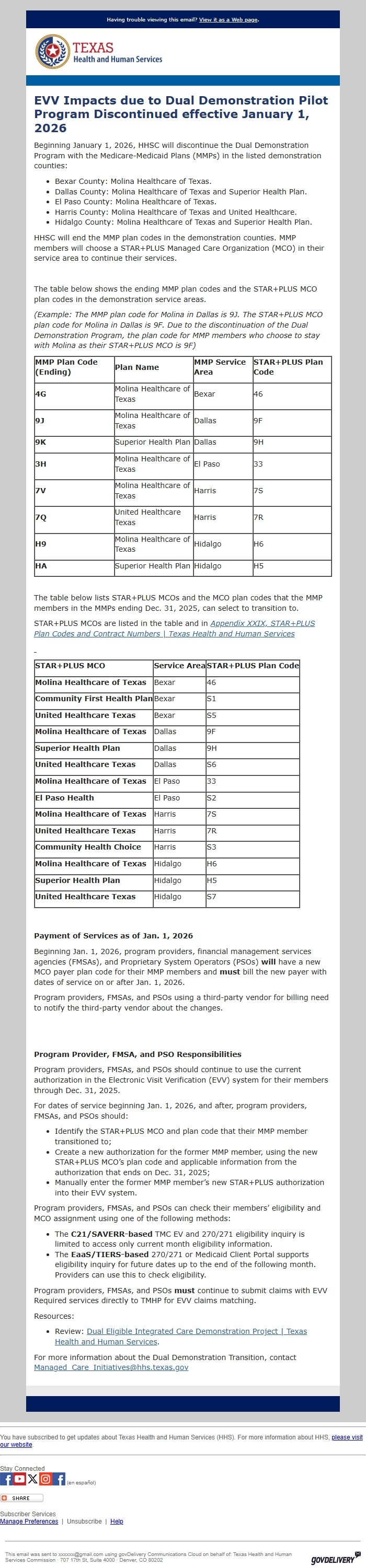
The table below shows the ending MMP plan codes and the STAR+PLUS MCO plan codes in the demonstration service areas.
"(Example: The MMP plan code for Molina in Dallas is 9J. The STAR+PLUS MCO plan code for Molina in Dallas is 9F. Due to the discontinuation of the Dual Demonstration Program, the plan code for MMP members who choose to stay with Molina as their STAR+PLUS MCO is 9F)"
*MMP Plan Code (Ending)*
*Plan Name*
*MMP Service Area*
*STAR+PLUS Plan Code*
*4G*
Molina Healthcare of Texas
Bexar
46
*9J*
Molina Healthcare of Texas
Dallas
9F
*9K*
Superior Health Plan
Dallas
9H
*3H*
Molina Healthcare of Texas
El Paso
33
*7V*
Molina Healthcare of Texas
Harris
7S
*7Q*
United Healthcare Texas
Harris
7R
*H9*
Molina Healthcare of Texas
Hidalgo
H6
*HA*
Superior Health Plan
Hidalgo
H5
The table below lists STAR+PLUS MCOs and the MCO plan codes that the MMP members in the MMPs ending Dec. 31, 2025, can select to transition to.
STAR+PLUS MCOs are listed in the table and in "Appendix XXIX, STAR+PLUS Plan Codes and Contract Numbers | Texas Health and Human Services" [ [link removed] ]__
"_ _"
*STAR+PLUS MCO*
*Service Area*
*STAR+PLUS Plan Code*
*Molina** Healthcare of Texas*
Bexar
46
*Community First Health Plan*
Bexar
S1
*United Healthcare Texas*
Bexar
S5
*Molina** Healthcare of Texas*
Dallas
9F
*Superior** Health Plan*
Dallas
9H
*United Healthcare Texas*
Dallas
S6
*Molina** Healthcare of Texas*
El Paso
33
*El Paso Health*
El Paso
S2
*Molina** Healthcare of Texas*
Harris
7S
*United Healthcare Texas*
Harris
7R
*Community Health Choice*
Harris
S3
*Molina** Healthcare of Texas*
Hidalgo
H6
*Superior** Health Plan*
Hidalgo
H5
*United Healthcare Texas*
Hidalgo
S7
* *
*Payment of Services as of Jan. 1, 2026*
Beginning Jan. 1, 2026, program providers, financial management services agencies (FMSAs), and Proprietary System Operators (PSOs) *will* have a new MCO payer plan code for their MMP members and *must* bill the new payer with dates of service on or after Jan. 1, 2026.
Program providers, FMSAs, and PSOs using a third-party vendor for billing need to notify the third-party vendor about the changes.
* *
* *
*Program Provider, FMSA, and PSO Responsibilities*
Program providers, FMSAs, and PSOs should continue to use the current authorization in the Electronic Visit Verification (EVV) system for their members through Dec. 31, 2025.
For dates of service beginning Jan. 1, 2026, and after, program providers, FMSAs, and PSOs should:
* Identify the STAR+PLUS MCO and plan code that their MMP member transitioned to;
* Create a new authorization for the former MMP member, using the new STAR+PLUS MCO’s plan code and applicable information from the authorization that ends on Dec. 31, 2025;
* Manually enter the former MMP member’s new STAR+PLUS authorization into their EVV system.
Program providers, FMSAs, and PSOs can check their members’ eligibility and MCO assignment using one of the following methods:
* The *C21/SAVERR-based* TMC EV and 270/271 eligibility inquiry is limited to access only current month eligibility information.
* The *EaaS/TIERS-based* 270/271 or Medicaid Client Portal supports eligibility inquiry for future dates up to the end of the following month. Providers can use this to check eligibility.
Program providers, FMSAs, and PSOs *must* continue to submit claims with EVV Required services directly to TMHP for EVV claims matching.
Resources:
* Review: Dual Eligible Integrated Care Demonstration Project | Texas Health and Human Services [ [link removed] ].
For more information about the Dual Demonstration Transition, contact [email protected]
________________________________________________________________________
You have subscribed to get updates about Texas Health and Human Services (HHS). For more information about HHS, please visit our website [ [link removed] ].
________________________________________________________________________
Stay Connected Visit us on Facebook [ [link removed] ] Visit us on YouTube [ [link removed] ] Visit us on X [ [link removed] ] Visit us on Instagram [ [link removed] ] Visit us on Facebook [ [link removed] ] (en español)
Bookmark and Share [ [link removed] ]
Subscriber Services
Manage Preferences [ [link removed] ] | Unsubscribe [ [link removed] ] | Help [ [link removed] ]
________________________________________________________________________
This email was sent to [email protected] using govDelivery Communications Cloud on behalf of: Texas Health and Human Services Commission · 707 17th St, Suite 4000 · Denver, CO 80202 GovDelivery logo [ [link removed] ]
body .abe-column-block { min-height: 5px; } table.gd_combo_table img {margin-left:10px; margin-right:10px;} table.gd_combo_table div.govd_image_display img, table.gd_combo_table td.gd_combo_image_cell img {margin-left:0px; margin-right:0px;} table.govd_hr {min-width: 100%;}
HHS Logo [ [link removed] ]
EVV Impacts due to Dual Demonstration Pilot Program Discontinued effective January 1, 2026
Beginning January 1, 2026, HHSC will discontinue the Dual Demonstration Program with the Medicare-Medicaid Plans (MMPs) in the listed demonstration counties:
* Bexar County: Molina Healthcare of Texas.
* Dallas County: Molina Healthcare of Texas and Superior Health Plan.
* El Paso County: Molina Healthcare of Texas.
* Harris County: Molina Healthcare of Texas and United Healthcare.
* Hidalgo County: Molina Healthcare of Texas and Superior Health Plan.
HHSC will end the MMP plan codes in the demonstration counties. MMP members will choose a STAR+PLUS Managed Care Organization (MCO) in their service area to continue their services.
The table below shows the ending MMP plan codes and the STAR+PLUS MCO plan codes in the demonstration service areas.
"(Example: The MMP plan code for Molina in Dallas is 9J. The STAR+PLUS MCO plan code for Molina in Dallas is 9F. Due to the discontinuation of the Dual Demonstration Program, the plan code for MMP members who choose to stay with Molina as their STAR+PLUS MCO is 9F)"
*MMP Plan Code (Ending)*
*Plan Name*
*MMP Service Area*
*STAR+PLUS Plan Code*
*4G*
Molina Healthcare of Texas
Bexar
46
*9J*
Molina Healthcare of Texas
Dallas
9F
*9K*
Superior Health Plan
Dallas
9H
*3H*
Molina Healthcare of Texas
El Paso
33
*7V*
Molina Healthcare of Texas
Harris
7S
*7Q*
United Healthcare Texas
Harris
7R
*H9*
Molina Healthcare of Texas
Hidalgo
H6
*HA*
Superior Health Plan
Hidalgo
H5
The table below lists STAR+PLUS MCOs and the MCO plan codes that the MMP members in the MMPs ending Dec. 31, 2025, can select to transition to.
STAR+PLUS MCOs are listed in the table and in "Appendix XXIX, STAR+PLUS Plan Codes and Contract Numbers | Texas Health and Human Services" [ [link removed] ]__
"_ _"
*STAR+PLUS MCO*
*Service Area*
*STAR+PLUS Plan Code*
*Molina** Healthcare of Texas*
Bexar
46
*Community First Health Plan*
Bexar
S1
*United Healthcare Texas*
Bexar
S5
*Molina** Healthcare of Texas*
Dallas
9F
*Superior** Health Plan*
Dallas
9H
*United Healthcare Texas*
Dallas
S6
*Molina** Healthcare of Texas*
El Paso
33
*El Paso Health*
El Paso
S2
*Molina** Healthcare of Texas*
Harris
7S
*United Healthcare Texas*
Harris
7R
*Community Health Choice*
Harris
S3
*Molina** Healthcare of Texas*
Hidalgo
H6
*Superior** Health Plan*
Hidalgo
H5
*United Healthcare Texas*
Hidalgo
S7
* *
*Payment of Services as of Jan. 1, 2026*
Beginning Jan. 1, 2026, program providers, financial management services agencies (FMSAs), and Proprietary System Operators (PSOs) *will* have a new MCO payer plan code for their MMP members and *must* bill the new payer with dates of service on or after Jan. 1, 2026.
Program providers, FMSAs, and PSOs using a third-party vendor for billing need to notify the third-party vendor about the changes.
* *
* *
*Program Provider, FMSA, and PSO Responsibilities*
Program providers, FMSAs, and PSOs should continue to use the current authorization in the Electronic Visit Verification (EVV) system for their members through Dec. 31, 2025.
For dates of service beginning Jan. 1, 2026, and after, program providers, FMSAs, and PSOs should:
* Identify the STAR+PLUS MCO and plan code that their MMP member transitioned to;
* Create a new authorization for the former MMP member, using the new STAR+PLUS MCO’s plan code and applicable information from the authorization that ends on Dec. 31, 2025;
* Manually enter the former MMP member’s new STAR+PLUS authorization into their EVV system.
Program providers, FMSAs, and PSOs can check their members’ eligibility and MCO assignment using one of the following methods:
* The *C21/SAVERR-based* TMC EV and 270/271 eligibility inquiry is limited to access only current month eligibility information.
* The *EaaS/TIERS-based* 270/271 or Medicaid Client Portal supports eligibility inquiry for future dates up to the end of the following month. Providers can use this to check eligibility.
Program providers, FMSAs, and PSOs *must* continue to submit claims with EVV Required services directly to TMHP for EVV claims matching.
Resources:
* Review: Dual Eligible Integrated Care Demonstration Project | Texas Health and Human Services [ [link removed] ].
For more information about the Dual Demonstration Transition, contact [email protected]
________________________________________________________________________
You have subscribed to get updates about Texas Health and Human Services (HHS). For more information about HHS, please visit our website [ [link removed] ].
________________________________________________________________________
Stay Connected Visit us on Facebook [ [link removed] ] Visit us on YouTube [ [link removed] ] Visit us on X [ [link removed] ] Visit us on Instagram [ [link removed] ] Visit us on Facebook [ [link removed] ] (en español)
Bookmark and Share [ [link removed] ]
Subscriber Services
Manage Preferences [ [link removed] ] | Unsubscribe [ [link removed] ] | Help [ [link removed] ]
________________________________________________________________________
This email was sent to [email protected] using govDelivery Communications Cloud on behalf of: Texas Health and Human Services Commission · 707 17th St, Suite 4000 · Denver, CO 80202 GovDelivery logo [ [link removed] ]
body .abe-column-block { min-height: 5px; } table.gd_combo_table img {margin-left:10px; margin-right:10px;} table.gd_combo_table div.govd_image_display img, table.gd_combo_table td.gd_combo_image_cell img {margin-left:0px; margin-right:0px;} table.govd_hr {min-width: 100%;}
Message Analysis
- Sender: Texas Health and Human Services Commission
- Political Party: n/a
- Country: United States
- State/Locality: Texas
- Office: n/a
-
Email Providers:
- govDelivery
