Email
The Connection: Marketplace Coverage at Risk Under Budget Bill; Reducing Medicaid Churn; State Impact of Ending Premium Tax Credits; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Marketplace Coverage at Risk Under Budget Bill; Reducing Medicaid Churn; State Impact of Ending Premium Tax Credits; and More |
| Date | June 16, 2025 7:53 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
June 16, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
Marketplace Coverage at Risk Under Budget Bill
Millions of Americans who buy their health insurance through the Affordable Care Act marketplaces could soon face higher costs, fewer protections, and new barriers to getting covered — all because of the budget bill now moving through Congress and the expiration of enhanced premium tax credits. The legislation would make it harder to get and keep coverage, increase premiums and out-of-pocket costs, and leave nearly 8.2 million more people uninsured by 2034. When combined with proposed cuts to Medicaid, these changes could raise the number of insured to more than 40 million, close to pre-ACA levels. If the bill becomes law, families could feel the effects as soon as this fall.
READ MORE ([link removed] )
Stabilizing Coverage for People with Medicaid
Because of fluctuations in their incomes and barriers they encounter in renewing their plans, many Americans with Medicaid endure a repeating cycle of losing and regaining coverage throughout the year. It’s a phenomenon known as “churn,” and it’s a costly one for both patients and states. In a new Commonwealth Fund issue brief, the George Washington University’s MaryBeth Musumeci and colleagues show how Medicaid churn can be reduced through better policy. They identify a number of strategies to improve the continuity of people’s Medicaid coverage, including ensuring uninterrupted Medicaid coverage for at least 12 months, switching to automatic coverage renewal, and providing in-person enrollment assistance.
READ MORE ([link removed] )
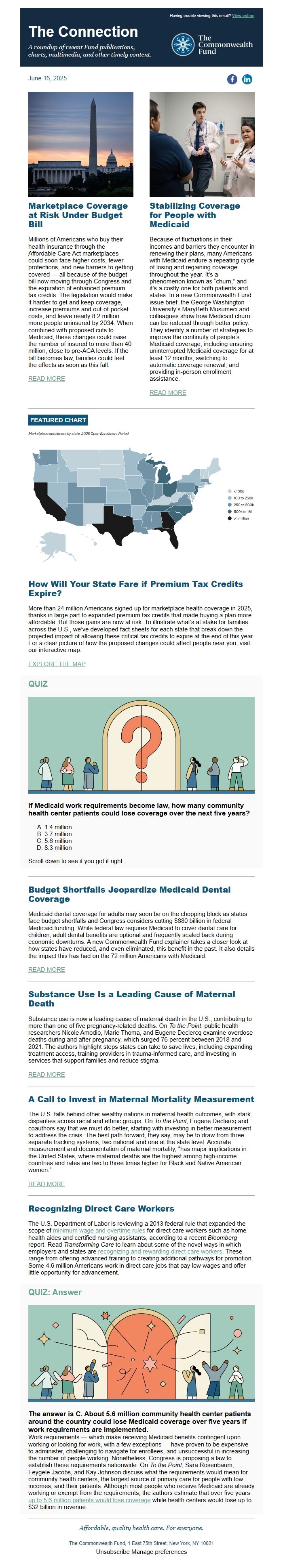
FEATURED CHART
How Will Your State Fare if Premium Tax Credits Expire?
More than 24 million Americans signed up for marketplace health coverage in 2025, thanks in large part to expanded premium tax credits that made buying a plan more affordable. But those gains are now at risk. To illustrate what’s at stake for families across the U.S., we’ve developed fact sheets for each state that break down the projected impact of allowing these critical tax credits to expire at the end of this year. For a clear picture of how the proposed changes could affect people near you, visit our interactive map.
EXPLORE THE MAP ([link removed] )
QUIZ
If Medicaid work requirements become law, how many community health center patients could lose coverage over the next five years?
- 1.4 million
- 3.7 million
- 5.6 million
- 8.3 million
Scroll down to see if you got it right.
Budget Shortfalls Jeopardize Medicaid Dental Coverage
Medicaid dental coverage for adults may soon be on the chopping block as states face budget shortfalls and Congress considers cutting $880 billion in federal Medicaid funding. While federal law requires Medicaid to cover dental care for children, adult dental benefits are optional and frequently scaled back during economic downturns. A new Commonwealth Fund explainer takes a closer look at how states have reduced, and even eliminated, this benefit in the past. It also details the impact this has had on the 72 million Americans with Medicaid.
READ MORE ([link removed] )
Substance Use Is a Leading Cause of Maternal Death
Substance use is now a leading cause of maternal death in the U.S., contributing to more than one of five pregnancy-related deaths. On To the Point, public health researchers Nicole Amodio, Marie Thoma, and Eugene Declercq examine overdose deaths during and after pregnancy, which surged 76 percent between 2018 and 2021. The authors highlight steps states can take to save lives, including expanding treatment access, training providers in trauma-informed care, and investing in services that support families and reduce stigma.
READ MORE ([link removed] )
A Call to Invest in Maternal Mortality Measurement
The U.S. falls behind other wealthy nations in maternal health outcomes, with stark disparities across racial and ethnic groups. On To the Point, Eugene Declercq and coauthors say that we must do better, starting with investing in better measurement to address the crisis. The best path forward, they say, may be to draw from three separate tracking systems, two national and one at the state level. Accurate measurement and documentation of maternal mortality, “has major implications in the United States, where maternal deaths are the highest among high-income countries and rates are two to three times higher for Black and Native American women.”
READ MORE ([link removed] )
Recognizing Direct Care Workers
The U.S. Department of Labor is reviewing a 2013 federal rule that expanded the scope of minimum wage and overtime rules ([link removed] ) for direct care workers such as home health aides and certified nursing assistants, according to a recent Bloomberg report. Read Transforming Care to learn about some of the novel ways in which employers and states are recognizing and rewarding direct care workers ([link removed] ) . These range from offering advanced training to creating additional pathways for promotion. Some 4.6 million Americans work in direct care jobs that pay low wages and offer little opportunity for advancement.
QUIZ: Answer
The answer is C. About 5.6 million community health center patients around the country could lose Medicaid coverage over five years if work requirements are implemented.
Work requirements — which make receiving Medicaid benefits contingent upon working or looking for work, with a few exceptions — have proven to be expensive to administer, challenging to navigate for enrollees, and unsuccessful in increasing the number of people working. Nonetheless, Congress is proposing a law to establish these requirements nationwide. On To the Point, Sara Rosenbaum, Feygele Jacobs, and Kay Johnson discuss what the requirements would mean for community health centers, the largest source of primary care for people with low incomes, and their patients. Although most people who receive Medicaid are already working or exempt from the requirements, the authors estimate that over five years up to 5.6 million patients would lose coverage ([link removed] ) while health centers would lose up to $32 billion in revenue.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
June 16, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
Marketplace Coverage at Risk Under Budget Bill
Millions of Americans who buy their health insurance through the Affordable Care Act marketplaces could soon face higher costs, fewer protections, and new barriers to getting covered — all because of the budget bill now moving through Congress and the expiration of enhanced premium tax credits. The legislation would make it harder to get and keep coverage, increase premiums and out-of-pocket costs, and leave nearly 8.2 million more people uninsured by 2034. When combined with proposed cuts to Medicaid, these changes could raise the number of insured to more than 40 million, close to pre-ACA levels. If the bill becomes law, families could feel the effects as soon as this fall.
READ MORE ([link removed] )
Stabilizing Coverage for People with Medicaid
Because of fluctuations in their incomes and barriers they encounter in renewing their plans, many Americans with Medicaid endure a repeating cycle of losing and regaining coverage throughout the year. It’s a phenomenon known as “churn,” and it’s a costly one for both patients and states. In a new Commonwealth Fund issue brief, the George Washington University’s MaryBeth Musumeci and colleagues show how Medicaid churn can be reduced through better policy. They identify a number of strategies to improve the continuity of people’s Medicaid coverage, including ensuring uninterrupted Medicaid coverage for at least 12 months, switching to automatic coverage renewal, and providing in-person enrollment assistance.
READ MORE ([link removed] )
FEATURED CHART
How Will Your State Fare if Premium Tax Credits Expire?
More than 24 million Americans signed up for marketplace health coverage in 2025, thanks in large part to expanded premium tax credits that made buying a plan more affordable. But those gains are now at risk. To illustrate what’s at stake for families across the U.S., we’ve developed fact sheets for each state that break down the projected impact of allowing these critical tax credits to expire at the end of this year. For a clear picture of how the proposed changes could affect people near you, visit our interactive map.
EXPLORE THE MAP ([link removed] )
QUIZ
If Medicaid work requirements become law, how many community health center patients could lose coverage over the next five years?
- 1.4 million
- 3.7 million
- 5.6 million
- 8.3 million
Scroll down to see if you got it right.
Budget Shortfalls Jeopardize Medicaid Dental Coverage
Medicaid dental coverage for adults may soon be on the chopping block as states face budget shortfalls and Congress considers cutting $880 billion in federal Medicaid funding. While federal law requires Medicaid to cover dental care for children, adult dental benefits are optional and frequently scaled back during economic downturns. A new Commonwealth Fund explainer takes a closer look at how states have reduced, and even eliminated, this benefit in the past. It also details the impact this has had on the 72 million Americans with Medicaid.
READ MORE ([link removed] )
Substance Use Is a Leading Cause of Maternal Death
Substance use is now a leading cause of maternal death in the U.S., contributing to more than one of five pregnancy-related deaths. On To the Point, public health researchers Nicole Amodio, Marie Thoma, and Eugene Declercq examine overdose deaths during and after pregnancy, which surged 76 percent between 2018 and 2021. The authors highlight steps states can take to save lives, including expanding treatment access, training providers in trauma-informed care, and investing in services that support families and reduce stigma.
READ MORE ([link removed] )
A Call to Invest in Maternal Mortality Measurement
The U.S. falls behind other wealthy nations in maternal health outcomes, with stark disparities across racial and ethnic groups. On To the Point, Eugene Declercq and coauthors say that we must do better, starting with investing in better measurement to address the crisis. The best path forward, they say, may be to draw from three separate tracking systems, two national and one at the state level. Accurate measurement and documentation of maternal mortality, “has major implications in the United States, where maternal deaths are the highest among high-income countries and rates are two to three times higher for Black and Native American women.”
READ MORE ([link removed] )
Recognizing Direct Care Workers
The U.S. Department of Labor is reviewing a 2013 federal rule that expanded the scope of minimum wage and overtime rules ([link removed] ) for direct care workers such as home health aides and certified nursing assistants, according to a recent Bloomberg report. Read Transforming Care to learn about some of the novel ways in which employers and states are recognizing and rewarding direct care workers ([link removed] ) . These range from offering advanced training to creating additional pathways for promotion. Some 4.6 million Americans work in direct care jobs that pay low wages and offer little opportunity for advancement.
QUIZ: Answer
The answer is C. About 5.6 million community health center patients around the country could lose Medicaid coverage over five years if work requirements are implemented.
Work requirements — which make receiving Medicaid benefits contingent upon working or looking for work, with a few exceptions — have proven to be expensive to administer, challenging to navigate for enrollees, and unsuccessful in increasing the number of people working. Nonetheless, Congress is proposing a law to establish these requirements nationwide. On To the Point, Sara Rosenbaum, Feygele Jacobs, and Kay Johnson discuss what the requirements would mean for community health centers, the largest source of primary care for people with low incomes, and their patients. Although most people who receive Medicaid are already working or exempt from the requirements, the authors estimate that over five years up to 5.6 million patients would lose coverage ([link removed] ) while health centers would lose up to $32 billion in revenue.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
