Email
The Connection: Out-of-Pocket Costs of Employer Insurance; Community Approaches to Improving Maternal Health; Making Health Care in ACA Plans More Affordable; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Out-of-Pocket Costs of Employer Insurance; Community Approaches to Improving Maternal Health; Making Health Care in ACA Plans More Affordable; and More |
| Date | March 24, 2025 8:44 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
March 24, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
Employer Insurance Can Strain Household Budgets
Employer-based insurance is the primary source of health coverage in the U.S. But out-of-pocket costs, from premium contributions and deductibles to copayments and coinsurance, can inflict a significant financial burden on workers and their families. On To the Point, Commonwealth Fund researchers look at the affordability of health insurance costs for workers. In comparing employee premium contributions and deductibles to median income in each state, they found significant variation in affordability across the country.
READ MORE ([link removed] )
Community-Driven Strategies to Improve Maternal Health
Recognizing that the U.S. maternal mortality crisis is largely preventable, legislators at the federal, state, and local levels are committed to addressing it. On To the Point, Anne Morris Reid and colleagues discuss the importance of partnering with communities and involving people with lived experience in these efforts. Drawing on findings from a forum with maternal health stakeholders that included policymakers, funders, and practitioners, the authors discuss recommendations for developing a national strategy that encompasses related social needs.
READ MORE ([link removed] )
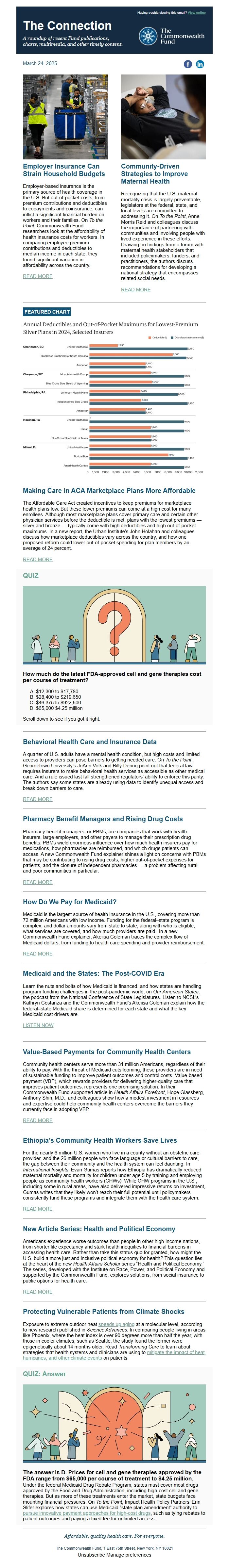
FEATURED CHART
Making Care in ACA Marketplace Plans More Affordable
The Affordable Care Act created incentives to keep premiums for marketplace health plans low. But these lower premiums can come at a high cost for many enrollees. Although most marketplace plans cover primary care and certain other physician services before the deductible is met, plans with the lowest premiums — silver and bronze — typically come with high deductibles and high out-of-pocket maximums. In a new report, the Urban Institute’s John Holahan and colleagues discuss how marketplace deductibles vary across the country, and how one proposed reform could lower out-of-pocket spending for plan members by an average of 24 percent.
READ MORE ([link removed] )
QUIZ
How much do the latest FDA-approved cell and gene therapies cost per course of treatment?
- $12,300 to $17,780
- $28,400 to $219,650
- $46,375 to $922,500
- $65,000 $4.25 million
Scroll down to see if you got it right.
Behavioral Health Care and Insurance Data
A quarter of U.S. adults have a mental health condition, but high costs and limited access to providers can pose barriers to getting needed care. On To the Point, Georgetown University’s JoAnn Volk and Billy Dering point out that federal law requires insurers to make behavioral health services as accessible as other medical care. And a rule issued last fall strengthened regulators’ ability to enforce this parity. The authors say some states are already using data to identify unequal access and break down barriers to care.
READ MORE ([link removed] )
Pharmacy Benefit Managers and Rising Drug Costs
Pharmacy benefit managers, or PBMs, are companies that work with health insurers, large employers, and other payers to manage their prescription drug benefits. PBMs wield enormous influence over how much health insurers pay for medications, how pharmacies are reimbursed, and which drugs patients can access. A new Commonwealth Fund explainer shines a light on concerns with PBMs that may be contributing to rising drug costs, higher out-of-pocket expenses for patients, and the closure of independent pharmacies — a problem affecting rural and poor communities in particular.
READ MORE ([link removed] )
How Do We Pay for Medicaid?
Medicaid is the largest source of health insurance in the U.S., covering more than 72 million Americans with low income. Funding for the federal–state program is complex, and dollar amounts vary from state to state, along with who is eligible, what services are covered, and how much providers are paid. In a new Commonwealth Fund explainer, Akeiisa Coleman traces the complex flow of Medicaid dollars, from funding to health care spending and provider reimbursement.
READ MORE ([link removed] )
Medicaid and the States: The Post-COVID Era
Learn the nuts and bolts of how Medicaid is financed, and how states are handling program funding challenges in the post-pandemic world, on Our American States, the podcast from the National Conference of State Legislatures. Listen to NCSL’s Kathryn Costanza and the Commonwealth Fund’s Akeiisa Coleman explain how the federal–state Medicaid share is determined for each state and what the key Medicaid cost drivers are.
LISTEN NOW ([link removed] )
Value-Based Payments for Community Health Centers
Community health centers serve more than 31 million Americans, regardless of their ability to pay. With the threat of Medicaid cuts looming, these providers are in need of sustainable funding to improve patient outcomes and control costs. Value-based payment (VBP), which rewards providers for delivering higher-quality care that improves patient outcomes, represents one promising solution. In their Commonwealth Fund-supported article in Health Affairs Forefront, Hope Glassberg, Anthony Shih, M.D., and colleagues show how a modest investment in resources and expertise could help community health centers overcome the barriers they currently face in adopting VBP.
READ MORE ([link removed] )
Ethiopia’s Community Health Workers Save Lives
For the nearly 6 million U.S. women who live in a county without an obstetric care provider, and the 26 million people who face language or cultural barriers to care, the gap between their community and the health system can feel daunting. In International Insights, Evan Gumas reports how Ethiopia has dramatically reduced maternal mortality and mortality for children under age 5 by training and employing people as community health workers (CHWs). While CHW programs in the U.S., including some in rural areas, have also delivered impressive returns on investment, Gumas writes that they likely won’t reach their full potential until policymakers consistently fund these programs and integrate them with the health care system.
READ MORE ([link removed] )
New Article Series: Health and Political Economy
Americans experience worse outcomes than people in other high-income nations, from shorter life expectancy and stark health inequities to financial burdens in accessing health care. Rather than take this status quo for granted, how might the U.S. build a more just and inclusive political economy for health? This question lies at the heart of the new Health Affairs Scholar series “Health and Political Economy.” The series, developed with the Institute on Race, Power, and Political Economy and supported by the Commonwealth Fund, explores solutions, from social insurance to public options for health care.
READ MORE ([link removed] )
Protecting Vulnerable Patients from Climate Shocks
Exposure to extreme outdoor heat speeds up aging ([link removed] ) at a molecular level, according to new research published in Science Advances. In comparing people living in areas like Phoenix, where the heat index is over 90 degrees more than half the year, with those in cooler climates, such as Seattle, the study found the former were epigenetically about 14 months older. Read Transforming Care to learn about strategies that health systems and clinicians are using to mitigate the impact of heat, hurricanes, and other climate events ([link removed] ) on patients.
QUIZ: Answer
The answer is D. Prices for cell and gene therapies approved by the FDA range from $65,000 per course of treatment to $4.25 million.
Under the federal Medicaid Drug Rebate Program, states must cover most drugs approved by the Food and Drug Administration, including high-cost cell and gene therapies. But as more of these treatments enter the market, state budgets face mounting financial pressures. On To the Point, Impact Health Policy Partners’ Erin Slifer explores how states can use Medicaid “state plan amendment” authority to pursue innovative payment approaches for high-cost drugs ([link removed] ) , such as tying rebates to patient outcomes and paying a fixed fee for unlimited access.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
March 24, 2025
Facebook ([link removed] )
LinkedIn ([link removed] )
Employer Insurance Can Strain Household Budgets
Employer-based insurance is the primary source of health coverage in the U.S. But out-of-pocket costs, from premium contributions and deductibles to copayments and coinsurance, can inflict a significant financial burden on workers and their families. On To the Point, Commonwealth Fund researchers look at the affordability of health insurance costs for workers. In comparing employee premium contributions and deductibles to median income in each state, they found significant variation in affordability across the country.
READ MORE ([link removed] )
Community-Driven Strategies to Improve Maternal Health
Recognizing that the U.S. maternal mortality crisis is largely preventable, legislators at the federal, state, and local levels are committed to addressing it. On To the Point, Anne Morris Reid and colleagues discuss the importance of partnering with communities and involving people with lived experience in these efforts. Drawing on findings from a forum with maternal health stakeholders that included policymakers, funders, and practitioners, the authors discuss recommendations for developing a national strategy that encompasses related social needs.
READ MORE ([link removed] )
FEATURED CHART
Making Care in ACA Marketplace Plans More Affordable
The Affordable Care Act created incentives to keep premiums for marketplace health plans low. But these lower premiums can come at a high cost for many enrollees. Although most marketplace plans cover primary care and certain other physician services before the deductible is met, plans with the lowest premiums — silver and bronze — typically come with high deductibles and high out-of-pocket maximums. In a new report, the Urban Institute’s John Holahan and colleagues discuss how marketplace deductibles vary across the country, and how one proposed reform could lower out-of-pocket spending for plan members by an average of 24 percent.
READ MORE ([link removed] )
QUIZ
How much do the latest FDA-approved cell and gene therapies cost per course of treatment?
- $12,300 to $17,780
- $28,400 to $219,650
- $46,375 to $922,500
- $65,000 $4.25 million
Scroll down to see if you got it right.
Behavioral Health Care and Insurance Data
A quarter of U.S. adults have a mental health condition, but high costs and limited access to providers can pose barriers to getting needed care. On To the Point, Georgetown University’s JoAnn Volk and Billy Dering point out that federal law requires insurers to make behavioral health services as accessible as other medical care. And a rule issued last fall strengthened regulators’ ability to enforce this parity. The authors say some states are already using data to identify unequal access and break down barriers to care.
READ MORE ([link removed] )
Pharmacy Benefit Managers and Rising Drug Costs
Pharmacy benefit managers, or PBMs, are companies that work with health insurers, large employers, and other payers to manage their prescription drug benefits. PBMs wield enormous influence over how much health insurers pay for medications, how pharmacies are reimbursed, and which drugs patients can access. A new Commonwealth Fund explainer shines a light on concerns with PBMs that may be contributing to rising drug costs, higher out-of-pocket expenses for patients, and the closure of independent pharmacies — a problem affecting rural and poor communities in particular.
READ MORE ([link removed] )
How Do We Pay for Medicaid?
Medicaid is the largest source of health insurance in the U.S., covering more than 72 million Americans with low income. Funding for the federal–state program is complex, and dollar amounts vary from state to state, along with who is eligible, what services are covered, and how much providers are paid. In a new Commonwealth Fund explainer, Akeiisa Coleman traces the complex flow of Medicaid dollars, from funding to health care spending and provider reimbursement.
READ MORE ([link removed] )
Medicaid and the States: The Post-COVID Era
Learn the nuts and bolts of how Medicaid is financed, and how states are handling program funding challenges in the post-pandemic world, on Our American States, the podcast from the National Conference of State Legislatures. Listen to NCSL’s Kathryn Costanza and the Commonwealth Fund’s Akeiisa Coleman explain how the federal–state Medicaid share is determined for each state and what the key Medicaid cost drivers are.
LISTEN NOW ([link removed] )
Value-Based Payments for Community Health Centers
Community health centers serve more than 31 million Americans, regardless of their ability to pay. With the threat of Medicaid cuts looming, these providers are in need of sustainable funding to improve patient outcomes and control costs. Value-based payment (VBP), which rewards providers for delivering higher-quality care that improves patient outcomes, represents one promising solution. In their Commonwealth Fund-supported article in Health Affairs Forefront, Hope Glassberg, Anthony Shih, M.D., and colleagues show how a modest investment in resources and expertise could help community health centers overcome the barriers they currently face in adopting VBP.
READ MORE ([link removed] )
Ethiopia’s Community Health Workers Save Lives
For the nearly 6 million U.S. women who live in a county without an obstetric care provider, and the 26 million people who face language or cultural barriers to care, the gap between their community and the health system can feel daunting. In International Insights, Evan Gumas reports how Ethiopia has dramatically reduced maternal mortality and mortality for children under age 5 by training and employing people as community health workers (CHWs). While CHW programs in the U.S., including some in rural areas, have also delivered impressive returns on investment, Gumas writes that they likely won’t reach their full potential until policymakers consistently fund these programs and integrate them with the health care system.
READ MORE ([link removed] )
New Article Series: Health and Political Economy
Americans experience worse outcomes than people in other high-income nations, from shorter life expectancy and stark health inequities to financial burdens in accessing health care. Rather than take this status quo for granted, how might the U.S. build a more just and inclusive political economy for health? This question lies at the heart of the new Health Affairs Scholar series “Health and Political Economy.” The series, developed with the Institute on Race, Power, and Political Economy and supported by the Commonwealth Fund, explores solutions, from social insurance to public options for health care.
READ MORE ([link removed] )
Protecting Vulnerable Patients from Climate Shocks
Exposure to extreme outdoor heat speeds up aging ([link removed] ) at a molecular level, according to new research published in Science Advances. In comparing people living in areas like Phoenix, where the heat index is over 90 degrees more than half the year, with those in cooler climates, such as Seattle, the study found the former were epigenetically about 14 months older. Read Transforming Care to learn about strategies that health systems and clinicians are using to mitigate the impact of heat, hurricanes, and other climate events ([link removed] ) on patients.
QUIZ: Answer
The answer is D. Prices for cell and gene therapies approved by the FDA range from $65,000 per course of treatment to $4.25 million.
Under the federal Medicaid Drug Rebate Program, states must cover most drugs approved by the Food and Drug Administration, including high-cost cell and gene therapies. But as more of these treatments enter the market, state budgets face mounting financial pressures. On To the Point, Impact Health Policy Partners’ Erin Slifer explores how states can use Medicaid “state plan amendment” authority to pursue innovative payment approaches for high-cost drugs ([link removed] ) , such as tying rebates to patient outcomes and paying a fixed fee for unlimited access.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
