Email
The Connection: Gun Violence in U.S. and Abroad; Protecting Consumers from Medical Debt; Enhancing Essential Health Benefits; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Gun Violence in U.S. and Abroad; Protecting Consumers from Medical Debt; Enhancing Essential Health Benefits; and More |
| Date | November 18, 2024 9:22 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
November 18, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
The Health Costs of U.S. Gun Violence
The United States has more firearm-related deaths than nearly any other country. Gun violence — declared a public health crisis by the U.S. surgeon general in June 2024 — is also the leading cause of death for children and a contributor to rising preventable mortality rates. In a series of charts, Commonwealth Fund researchers illustrate how gun-related deaths in the U.S. compare with other countries and territories around the world. They show that virtually every U.S. state has a higher firearm mortality rate than most other countries.
READ MORE ([link removed] )
How States Protect People from Medical Debt
One in seven working-age Americans has fallen behind on paying their medical bills. Medical debt can discourage people from seeking the health care they need and interfere with their ability to afford basic necessities. Federal law requires hospitals to establish financial assistance policies and determine patient eligibility before engaging in “extraordinary collection actions,” but these mandates have had limited impact. On To the Point, Urban Institute researchers Michael Karpman and Fredric Blavin share their findings from four states with comprehensive medical debt legislation and offer key takeaways for other states considering similar efforts.
READ MORE ([link removed] )
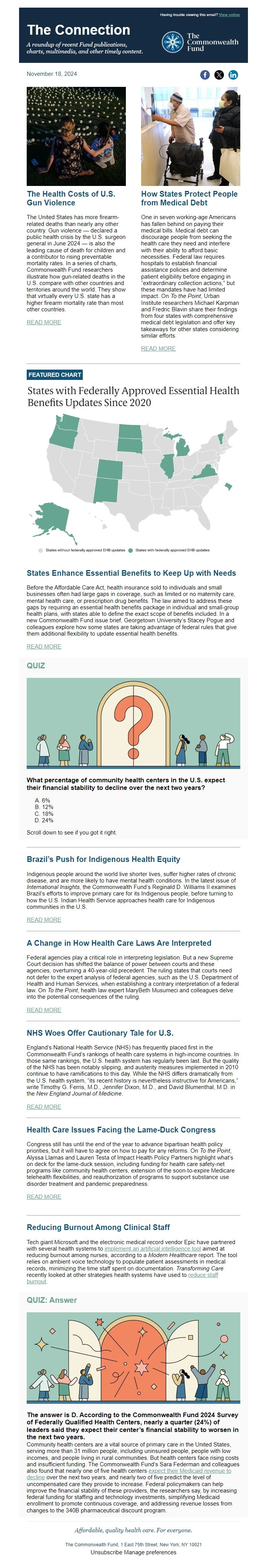
FEATURED CHART
States Enhance Essential Benefits to Keep Up with Needs
Before the Affordable Care Act, health insurance sold to individuals and small businesses often had large gaps in coverage, such as limited or no maternity care, mental health care, or prescription drug benefits. The law aimed to address these gaps by requiring an essential health benefits package in individual and small-group health plans, with states able to define the exact scope of benefits included. In a new Commonwealth Fund issue brief, Georgetown University’s Stacey Pogue and colleagues explore how some states are taking advantage of federal rules that give them additional flexibility to update essential health benefits.
READ MORE ([link removed] )
QUIZ
What percentage of community health centers in the U.S. expect their financial stability to decline over the next two years?
- 6%
- 12%
- 18%
- 24%
Scroll down to see if you got it right.
Brazil’s Push for Indigenous Health Equity
Indigenous people around the world live shorter lives, suffer higher rates of chronic disease, and are more likely to have mental health conditions. In the latest issue of International Insights, the Commonwealth Fund’s Reginald D. Williams II examines Brazil’s efforts to improve primary care for its Indigenous people, before turning to how the U.S. Indian Health Service approaches health care for Indigenous communities in the U.S.
READ MORE ([link removed] )
A Change in How Health Care Laws Are Interpreted
Federal agencies play a critical role in interpreting legislation. But a new Supreme Court decision has shifted the balance of power between courts and these agencies, overturning a 40-year-old precedent. The ruling states that courts need not defer to the expert analysis of federal agencies, such as the U.S. Department of Health and Human Services, when establishing a contrary interpretation of a federal law. On To the Point, health law expert MaryBeth Musumeci and colleagues delve into the potential consequences of the ruling.
READ MORE ([link removed] )
NHS Woes Offer Cautionary Tale for U.S.
England’s National Health Service (NHS) has frequently placed first in the Commonwealth Fund’s rankings of health care systems in high-income countries. In those same rankings, the U.S. health system has regularly been last. But the quality of the NHS has been notably slipping, and austerity measures implemented in 2010 continue to have ramifications to this day. While the NHS differs dramatically from the U.S. health system, “its recent history is nevertheless instructive for Americans,” write Timothy G. Ferris, M.D., Jennifer Dixon, M.D., and David Blumenthal, M.D. in the New England Journal of Medicine.
READ MORE ([link removed] )
Health Care Issues Facing the Lame-Duck Congress
Congress still has until the end of the year to advance bipartisan health policy priorities, but it will have to agree on how to pay for any reforms. On To the Point, Alyssa Llamas and Lauren Testa of Impact Health Policy Partners highlight what’s on deck for the lame-duck session, including funding for health care safety-net programs like community health centers, extension of the soon-to-expire Medicare telehealth flexibilities, and reauthorization of programs to support substance use disorder treatment and pandemic preparedness.
READ MORE ([link removed] )
Reducing Burnout Among Clinical Staff
Tech giant Microsoft and the electronic medical record vendor Epic have partnered with several health systems to implement an artificial intelligence tool ([link removed] ) aimed at reducing burnout among nurses, according to a Modern Healthcare report. The tool relies on ambient voice technology to populate patient assessments in medical records, minimizing the time staff spent on documentation. Transforming Care recently looked at other strategies health systems have used to reduce staff burnout ([link removed] ) .
QUIZ: Answer
The answer is D. According to the Commonwealth Fund 2024 Survey of Federally Qualified Health Centers, nearly a quarter (24%) of leaders said they expect their center’s financial stability to worsen in the next two years.
Community health centers are a vital source of primary care in the United States, serving more than 31 million people, including uninsured people, people with low incomes, and people living in rural communities. But health centers face rising costs and insufficient funding. The Commonwealth Fund’s Sara Federman and colleagues also found that nearly one of five health centers expect their Medicaid revenue to decline ([link removed] ) over the next two years, and nearly two of five predict the level of uncompensated care they provide to increase. Federal policymakers can help improve the financial stability of these providers, the researchers say, by increasing federal funding for staffing and technology investments, simplifying Medicaid enrollment to promote continuous coverage, and addressing revenue losses from changes to the 340B pharmaceutical discount program.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
November 18, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
The Health Costs of U.S. Gun Violence
The United States has more firearm-related deaths than nearly any other country. Gun violence — declared a public health crisis by the U.S. surgeon general in June 2024 — is also the leading cause of death for children and a contributor to rising preventable mortality rates. In a series of charts, Commonwealth Fund researchers illustrate how gun-related deaths in the U.S. compare with other countries and territories around the world. They show that virtually every U.S. state has a higher firearm mortality rate than most other countries.
READ MORE ([link removed] )
How States Protect People from Medical Debt
One in seven working-age Americans has fallen behind on paying their medical bills. Medical debt can discourage people from seeking the health care they need and interfere with their ability to afford basic necessities. Federal law requires hospitals to establish financial assistance policies and determine patient eligibility before engaging in “extraordinary collection actions,” but these mandates have had limited impact. On To the Point, Urban Institute researchers Michael Karpman and Fredric Blavin share their findings from four states with comprehensive medical debt legislation and offer key takeaways for other states considering similar efforts.
READ MORE ([link removed] )
FEATURED CHART
States Enhance Essential Benefits to Keep Up with Needs
Before the Affordable Care Act, health insurance sold to individuals and small businesses often had large gaps in coverage, such as limited or no maternity care, mental health care, or prescription drug benefits. The law aimed to address these gaps by requiring an essential health benefits package in individual and small-group health plans, with states able to define the exact scope of benefits included. In a new Commonwealth Fund issue brief, Georgetown University’s Stacey Pogue and colleagues explore how some states are taking advantage of federal rules that give them additional flexibility to update essential health benefits.
READ MORE ([link removed] )
QUIZ
What percentage of community health centers in the U.S. expect their financial stability to decline over the next two years?
- 6%
- 12%
- 18%
- 24%
Scroll down to see if you got it right.
Brazil’s Push for Indigenous Health Equity
Indigenous people around the world live shorter lives, suffer higher rates of chronic disease, and are more likely to have mental health conditions. In the latest issue of International Insights, the Commonwealth Fund’s Reginald D. Williams II examines Brazil’s efforts to improve primary care for its Indigenous people, before turning to how the U.S. Indian Health Service approaches health care for Indigenous communities in the U.S.
READ MORE ([link removed] )
A Change in How Health Care Laws Are Interpreted
Federal agencies play a critical role in interpreting legislation. But a new Supreme Court decision has shifted the balance of power between courts and these agencies, overturning a 40-year-old precedent. The ruling states that courts need not defer to the expert analysis of federal agencies, such as the U.S. Department of Health and Human Services, when establishing a contrary interpretation of a federal law. On To the Point, health law expert MaryBeth Musumeci and colleagues delve into the potential consequences of the ruling.
READ MORE ([link removed] )
NHS Woes Offer Cautionary Tale for U.S.
England’s National Health Service (NHS) has frequently placed first in the Commonwealth Fund’s rankings of health care systems in high-income countries. In those same rankings, the U.S. health system has regularly been last. But the quality of the NHS has been notably slipping, and austerity measures implemented in 2010 continue to have ramifications to this day. While the NHS differs dramatically from the U.S. health system, “its recent history is nevertheless instructive for Americans,” write Timothy G. Ferris, M.D., Jennifer Dixon, M.D., and David Blumenthal, M.D. in the New England Journal of Medicine.
READ MORE ([link removed] )
Health Care Issues Facing the Lame-Duck Congress
Congress still has until the end of the year to advance bipartisan health policy priorities, but it will have to agree on how to pay for any reforms. On To the Point, Alyssa Llamas and Lauren Testa of Impact Health Policy Partners highlight what’s on deck for the lame-duck session, including funding for health care safety-net programs like community health centers, extension of the soon-to-expire Medicare telehealth flexibilities, and reauthorization of programs to support substance use disorder treatment and pandemic preparedness.
READ MORE ([link removed] )
Reducing Burnout Among Clinical Staff
Tech giant Microsoft and the electronic medical record vendor Epic have partnered with several health systems to implement an artificial intelligence tool ([link removed] ) aimed at reducing burnout among nurses, according to a Modern Healthcare report. The tool relies on ambient voice technology to populate patient assessments in medical records, minimizing the time staff spent on documentation. Transforming Care recently looked at other strategies health systems have used to reduce staff burnout ([link removed] ) .
QUIZ: Answer
The answer is D. According to the Commonwealth Fund 2024 Survey of Federally Qualified Health Centers, nearly a quarter (24%) of leaders said they expect their center’s financial stability to worsen in the next two years.
Community health centers are a vital source of primary care in the United States, serving more than 31 million people, including uninsured people, people with low incomes, and people living in rural communities. But health centers face rising costs and insufficient funding. The Commonwealth Fund’s Sara Federman and colleagues also found that nearly one of five health centers expect their Medicaid revenue to decline ([link removed] ) over the next two years, and nearly two of five predict the level of uncompensated care they provide to increase. Federal policymakers can help improve the financial stability of these providers, the researchers say, by increasing federal funding for staffing and technology investments, simplifying Medicaid enrollment to promote continuous coverage, and addressing revenue losses from changes to the 340B pharmaceutical discount program.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
