Email
The Connection: U.S. Ranks Last in 10-Nation Study; How the Election Could Affect Coverage; What Happens If ACA Tax Credits Expire; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: U.S. Ranks Last in 10-Nation Study; How the Election Could Affect Coverage; What Happens If ACA Tax Credits Expire; and More |
| Date | October 1, 2024 9:14 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
October 1, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
U.S. Health Care System Ranks Last in 10-Nation Study
The U.S. health care system is failing to keep Americans healthy, ranking last in a Commonwealth Fund report that compares health and health care in 10 countries. U.S. performance is particularly poor when it comes to health equity, access to care, efficiency, and health outcomes. According to Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System, the U.S. spends the most on health care, yet Americans live shorter, less healthy lives than people in the nine other study countries. “The U.S. continues to be in a class by itself in the underperformance of its health care sector,” say the study’s authors, who call for policymakers and health care leaders to learn from other countries’ experiences and act.
READ MORE ([link removed] )
How Could the Fall Election Affect Health Care Coverage?
The next president has the power to either protect and build on recent gains in health coverage or return to policies that can lead to higher uninsured rates, high premiums and out-of-pocket costs, and rising medical debt. In the latest explainer in our special series What’s at Stake in the 2024 Election, we look at how this fall’s election could affect people’s health insurance coverage. A Harris administration would likely continue efforts to reduce health plan premiums and expand coverage while protecting consumers from medical debt. A second Trump administration would likely loosen regulations and try to reduce health spending in ways that could make it more difficult for people to afford coverage.
READ MORE ([link removed] )
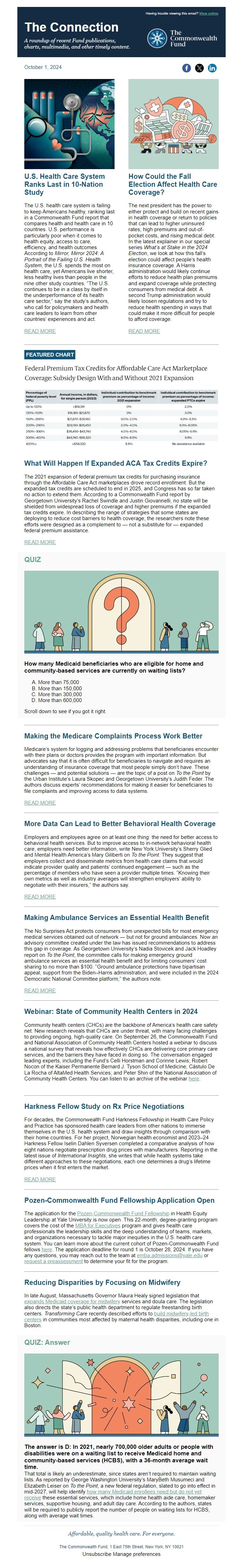
FEATURED CHART
What Will Happen If Expanded ACA Tax Credits Expire?
The 2021 expansion of federal premium tax credits for purchasing insurance through the Affordable Care Act marketplaces drove record enrollment. But the expanded tax credits are scheduled to end in 2025, and Congress has so far taken no action to extend them. According to a Commonwealth Fund report by Georgetown University’s Rachel Swindle and Justin Giovannelli, no state will be shielded from widespread loss of coverage and higher premiums if the expanded tax credits expire. In describing the range of strategies that some states are deploying to reduce cost barriers to health coverage, the researchers note these efforts were designed as a complement to — not a substitute for — expanded federal premium assistance.
READ MORE ([link removed] )
QUIZ
How many Medicaid beneficiaries who are eligible for home and community-based services are currently on waiting lists?
- More than 75,000
- More than 150,000
- More than 300,000
- More than 600,000
Scroll down to see if you got it right.
Making the Medicare Complaints Process Work Better
Medicare’s system for logging and addressing problems that beneficiaries encounter with their plans or doctors provides the program with important information. But advocates say that it is often difficult for beneficiaries to navigate and requires an understanding of insurance coverage that most people simply don’t have. These challenges — and potential solutions — are the topic of a post on To the Point by the Urban Institute’s Laura Skopec and Georgetown University’s Judith Feder. The authors discuss experts’ recommendations for making it easier for beneficiaries to file complaints and improving access to data systems.
READ MORE ([link removed] )
More Data Can Lead to Better Behavioral Health Coverage
Employers and employees agree on at least one thing: the need for better access to behavioral health services. But to improve access to in-network behavioral health care, employers need better information, write New York University’s Sherry Glied and Mental Health America’s Mary Giliberti on To the Point. They suggest that employers collect and disseminate metrics from health care claims that would indicate provider quality and patients’ continued engagement — such as the percentage of members who have seen a provider multiple times. “Knowing their own metrics as well as industry averages will strengthen employers’ ability to negotiate with their insurers,” the authors say.
READ MORE ([link removed] )
Making Ambulance Services an Essential Health Benefit
The No Surprises Act protects consumers from unexpected bills for most emergency medical services obtained out of network — but not for ground ambulances. Now an advisory committee created under the law has issued recommendations to address this gap in coverage. As Georgetown University’s Nadia Stovicek and Jack Hoadley report on To the Point, the committee calls for making emergency ground ambulance services an essential health benefit and for limiting consumers’ cost sharing to no more than $100. “Ground ambulance protections have bipartisan appeal, support from the Biden–Harris administration, and were included in the 2024 Democratic National Committee platform,” the authors note.
READ MORE ([link removed] )
Webinar: State of Community Health Centers in 2024
Community health centers (CHCs) are the backbone of America’s health care safety net. New research reveals that CHCs are under threat, with many facing challenges to providing ongoing, high-quality care. On September 26, the Commonwealth Fund and National Association of Community Health Centers hosted a webinar to discuss a national survey that reveals how effectively CHCs are delivering core primary care services, and the barriers they have faced in doing so. The conversation engaged leading experts, including the Fund’s Celli Horstman and Corinne Lewis; Robert Nocon of the Kaiser Permanente Bernard J. Tyson School of Medicine; Cástulo De La Rocha of AltaMed Health Services; and Peter Shin of the National Association of Community Health Centers. You can listen to an archive of the webinar here ([link removed] ) .
Harkness Fellow Study on Rx Price Negotiations
For decades, the Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice has sponsored health care leaders from other nations to immerse themselves in the U.S. health system and draw insights through comparison with their home countries. For her project, Norwegian health economist and 2023–24 Harkness Fellow Iselin Dahlen Syversen completed a comparative analysis of how eight nations negotiate prescription drug prices with manufacturers. Reporting in the latest issue of International Insights, she writes that while health systems take different approaches to these negotiations, each one determines a drug’s lifetime prices when it first enters the market.
READ MORE ([link removed] )
Pozen-Commonwealth Fund Fellowship Application Open
The application for the Pozen-Commonwealth Fund Fellowship ([link removed] ) in Health Equity Leadership at Yale University is now open. This 22-month, degree-granting program covers the cost of the MBA for Executives ([link removed] ) program and gives health care professionals the leadership skills and the deep understanding of teams, markets, and organizations necessary to tackle major inequities in the U.S. health care system. You can learn more about the current cohort of Pozen-Commonwealth Fund fellows here ([link removed] ) . The application deadline for round 1 is October 28, 2024. If you have any questions, you may reach out to the team at [email protected] (mailto:[email protected]) or request a preassessment ([link removed] ) to determine your fit for the program.
Reducing Disparities by Focusing on Midwifery
In late August, Massachusetts Governor Maura Healy signed legislation that expands Medicaid coverage for midwifery ([link removed] ) services and doula care. The legislation also directs the state’s public health department to regulate freestanding birth centers. Transforming Care recently described efforts to build midwifery-led birth centers ([link removed] ) in communities most affected by maternal health disparities, including one in Boston.
QUIZ: Answer
The answer is D: In 2021, nearly 700,000 older adults or people with disabilities were on a waiting list to receive Medicaid home and community-based services (HCBS), with a 36-month average wait time.
That total is likely an underestimate, since states aren’t required to maintain waiting lists. As reported by George Washington University’s MaryBeth Musumeci and Elizabeth Leiser on To the Point, a new federal regulation, slated to go into effect in mid-2027, will help identify how many Medicaid enrollees need but do not yet receive ([link removed] ) these essential services, which include home health aide care, homemaker services, supportive housing, and adult day care. According to the authors, states will be required to publicly report the number of people on waiting lists for HCBS, along with average wait times.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
October 1, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
U.S. Health Care System Ranks Last in 10-Nation Study
The U.S. health care system is failing to keep Americans healthy, ranking last in a Commonwealth Fund report that compares health and health care in 10 countries. U.S. performance is particularly poor when it comes to health equity, access to care, efficiency, and health outcomes. According to Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System, the U.S. spends the most on health care, yet Americans live shorter, less healthy lives than people in the nine other study countries. “The U.S. continues to be in a class by itself in the underperformance of its health care sector,” say the study’s authors, who call for policymakers and health care leaders to learn from other countries’ experiences and act.
READ MORE ([link removed] )
How Could the Fall Election Affect Health Care Coverage?
The next president has the power to either protect and build on recent gains in health coverage or return to policies that can lead to higher uninsured rates, high premiums and out-of-pocket costs, and rising medical debt. In the latest explainer in our special series What’s at Stake in the 2024 Election, we look at how this fall’s election could affect people’s health insurance coverage. A Harris administration would likely continue efforts to reduce health plan premiums and expand coverage while protecting consumers from medical debt. A second Trump administration would likely loosen regulations and try to reduce health spending in ways that could make it more difficult for people to afford coverage.
READ MORE ([link removed] )
FEATURED CHART
What Will Happen If Expanded ACA Tax Credits Expire?
The 2021 expansion of federal premium tax credits for purchasing insurance through the Affordable Care Act marketplaces drove record enrollment. But the expanded tax credits are scheduled to end in 2025, and Congress has so far taken no action to extend them. According to a Commonwealth Fund report by Georgetown University’s Rachel Swindle and Justin Giovannelli, no state will be shielded from widespread loss of coverage and higher premiums if the expanded tax credits expire. In describing the range of strategies that some states are deploying to reduce cost barriers to health coverage, the researchers note these efforts were designed as a complement to — not a substitute for — expanded federal premium assistance.
READ MORE ([link removed] )
QUIZ
How many Medicaid beneficiaries who are eligible for home and community-based services are currently on waiting lists?
- More than 75,000
- More than 150,000
- More than 300,000
- More than 600,000
Scroll down to see if you got it right.
Making the Medicare Complaints Process Work Better
Medicare’s system for logging and addressing problems that beneficiaries encounter with their plans or doctors provides the program with important information. But advocates say that it is often difficult for beneficiaries to navigate and requires an understanding of insurance coverage that most people simply don’t have. These challenges — and potential solutions — are the topic of a post on To the Point by the Urban Institute’s Laura Skopec and Georgetown University’s Judith Feder. The authors discuss experts’ recommendations for making it easier for beneficiaries to file complaints and improving access to data systems.
READ MORE ([link removed] )
More Data Can Lead to Better Behavioral Health Coverage
Employers and employees agree on at least one thing: the need for better access to behavioral health services. But to improve access to in-network behavioral health care, employers need better information, write New York University’s Sherry Glied and Mental Health America’s Mary Giliberti on To the Point. They suggest that employers collect and disseminate metrics from health care claims that would indicate provider quality and patients’ continued engagement — such as the percentage of members who have seen a provider multiple times. “Knowing their own metrics as well as industry averages will strengthen employers’ ability to negotiate with their insurers,” the authors say.
READ MORE ([link removed] )
Making Ambulance Services an Essential Health Benefit
The No Surprises Act protects consumers from unexpected bills for most emergency medical services obtained out of network — but not for ground ambulances. Now an advisory committee created under the law has issued recommendations to address this gap in coverage. As Georgetown University’s Nadia Stovicek and Jack Hoadley report on To the Point, the committee calls for making emergency ground ambulance services an essential health benefit and for limiting consumers’ cost sharing to no more than $100. “Ground ambulance protections have bipartisan appeal, support from the Biden–Harris administration, and were included in the 2024 Democratic National Committee platform,” the authors note.
READ MORE ([link removed] )
Webinar: State of Community Health Centers in 2024
Community health centers (CHCs) are the backbone of America’s health care safety net. New research reveals that CHCs are under threat, with many facing challenges to providing ongoing, high-quality care. On September 26, the Commonwealth Fund and National Association of Community Health Centers hosted a webinar to discuss a national survey that reveals how effectively CHCs are delivering core primary care services, and the barriers they have faced in doing so. The conversation engaged leading experts, including the Fund’s Celli Horstman and Corinne Lewis; Robert Nocon of the Kaiser Permanente Bernard J. Tyson School of Medicine; Cástulo De La Rocha of AltaMed Health Services; and Peter Shin of the National Association of Community Health Centers. You can listen to an archive of the webinar here ([link removed] ) .
Harkness Fellow Study on Rx Price Negotiations
For decades, the Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice has sponsored health care leaders from other nations to immerse themselves in the U.S. health system and draw insights through comparison with their home countries. For her project, Norwegian health economist and 2023–24 Harkness Fellow Iselin Dahlen Syversen completed a comparative analysis of how eight nations negotiate prescription drug prices with manufacturers. Reporting in the latest issue of International Insights, she writes that while health systems take different approaches to these negotiations, each one determines a drug’s lifetime prices when it first enters the market.
READ MORE ([link removed] )
Pozen-Commonwealth Fund Fellowship Application Open
The application for the Pozen-Commonwealth Fund Fellowship ([link removed] ) in Health Equity Leadership at Yale University is now open. This 22-month, degree-granting program covers the cost of the MBA for Executives ([link removed] ) program and gives health care professionals the leadership skills and the deep understanding of teams, markets, and organizations necessary to tackle major inequities in the U.S. health care system. You can learn more about the current cohort of Pozen-Commonwealth Fund fellows here ([link removed] ) . The application deadline for round 1 is October 28, 2024. If you have any questions, you may reach out to the team at [email protected] (mailto:[email protected]) or request a preassessment ([link removed] ) to determine your fit for the program.
Reducing Disparities by Focusing on Midwifery
In late August, Massachusetts Governor Maura Healy signed legislation that expands Medicaid coverage for midwifery ([link removed] ) services and doula care. The legislation also directs the state’s public health department to regulate freestanding birth centers. Transforming Care recently described efforts to build midwifery-led birth centers ([link removed] ) in communities most affected by maternal health disparities, including one in Boston.
QUIZ: Answer
The answer is D: In 2021, nearly 700,000 older adults or people with disabilities were on a waiting list to receive Medicaid home and community-based services (HCBS), with a 36-month average wait time.
That total is likely an underestimate, since states aren’t required to maintain waiting lists. As reported by George Washington University’s MaryBeth Musumeci and Elizabeth Leiser on To the Point, a new federal regulation, slated to go into effect in mid-2027, will help identify how many Medicaid enrollees need but do not yet receive ([link removed] ) these essential services, which include home health aide care, homemaker services, supportive housing, and adult day care. According to the authors, states will be required to publicly report the number of people on waiting lists for HCBS, along with average wait times.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
