| |||
| |||
The government, pharmaceutical, and insurance companies have a system in place that financially incentivizes physicians to vaccinate kids. This is why pediatricians are dropping children who aren't fully vaccinated from their practices. |
Doctors Cash In: The Hidden Profits Behind Pediatric Vaccinations
Have you ever wondered why your pediatrician dropped your child from their practice and what may be driving the push to vaccinate kids at all costs?
By Megan Redshaw
Healthcare providers for years have been leading the charge in recommending—and often pressuring—parents to vaccinate their children. During the COVID-19 pandemic, strong endorsements from pediatricians played a significant role in the acceptance of experimental COVID-19 shots for kids, while parents expressed dismay at receiving dismissal letters for delaying or refusing a barrage of shots.
What these letters failed to disclose is that many pediatric practices lose out on financial rewards, including bonuses, if a certain percentage of their patient population isn’t vaccinated, and dismissal policies are one of many strategies used to increase vaccine compliance. If it were about public health, no physician would leave a child without established medical care based on whether a parent exercises their fundamental right to withhold consent to vaccination.
In a 2020 research letter published in JAMA Network, 51% of pediatricians reported that their office had a dismissal policy for families who refused vaccines in the primary series, while 37% of physicians reported often or always dismissing patients themselves. Eighteen percent of those surveyed said parents often or always changed their minds and agreed to vaccination when threatened with a dismissal policy.
What’s not disclosed to parents is that physicians are paid to vaccinate kids and receive performance-based incentives for having a certain percentage of their patient population vaccinated. The more vaccines they give, the more money they make. These incentives include direct bonuses and enhanced reimbursement rates provided by the government, pharmaceutical companies, and insurance companies—all geared toward maximizing vaccination rates.
Whether a physician works with privately insured patients or those who have insurance through the state, they are incentivized by the government to give as many vaccine doses as possible. In fact, reimbursement with private insurance is higher when a child receives more than three vaccine doses at their well visit, financially incentivizing doctors to administer as many vaccine doses as possible and could explain why even parents who selectively vaccinate receive pushback.
According to pediatrician Dr. Robert Zayjac, if everybody in his clinic followed the Centers for Disease Control and Prevention’s (CDC) schedule for vaccines and wellness visits, a physician would make $1.5 million.
CDC Program Creates Financial Incentives to Vaccinate
The CDC incentivizes physicians to vaccinate as many children as possible with as many vaccines as possible through its Vaccines for Children (VFC) program. The VFC is a federally funded program that provides vaccines at no cost to eligible children who might not otherwise be vaccinated due to an inability to pay.
The CDC buys vaccines at a discount from pharmaceutical companies and distributes them to state health departments, who then distribute them at no charge to healthcare providers enrolled in the program. This reduces up-front costs because physicians do not have to pay to purchase vaccines for eligible children.
Healthcare providers who enroll in the CDC’s program must comply with the agency’s recommended vaccination schedules, dosages, and contraindications established by the CDC’s Advisory Committee on Immunization Practices (ACIP), and must offer all age-appropriate vaccines. Medical practices are also encouraged to hire a staff member to promote vaccines.
Although the VFC program does not directly compensate physicians for providing vaccines, it offers significant financial incentives. For example, physicians can charge fees associated with a vaccination appointment, such as an administration fee for each vaccine administered through the program, an office visit fee, and costs for non-vaccine services during a vaccination appointment. For those on Medicaid, doctors bill the state for reimbursement.
The administration fees contribute to a physician's revenue, especially in practices where a large proportion of patients are eligible for VFC vaccines. Additionally, participating in the VFC program can help practices maintain high vaccination rates, which may be linked to other financial incentives, such as those provided by insurance companies.
Although the VFC program might seem like a noble cause on its face, it can inadvertently lead physicians to overlook potential vaccine risks in favor of meeting performance targets. By providing vaccines at no cost to practices and offering incentives tied to high vaccination rates, the VFC creates a financial environment where doctors are rewarded for administering as many vaccines as possible.
This performance-based system can pressure physicians to prioritize hitting vaccination targets over thoroughly evaluating the individual risks and benefits of vaccines for each child. As a result, the focus shifts from personalized patient care to maximizing vaccine numbers, potentially compromising the careful consideration of vaccine safety in the process.
In 2020 and 2021, the CDC’s funding for the VFC program totaled more than $4.5 billion and $3.8 billion, respectively, for purchasing vaccines and program operations. However, a 2023 audit by the Office of Inspector General found that the agency failed to ensure providers complied with vaccine storage and handling requirements, failed to conduct site visits, and did not follow up on compliance issues.
Insurance Companies Give Bonuses to Physicians to Push Vaccines
It’s not just government programs that offer financial incentives for high vaccination rates. Some insurance companies provide reimbursement and offer bonuses for reaching specific vaccination targets among patient populations.
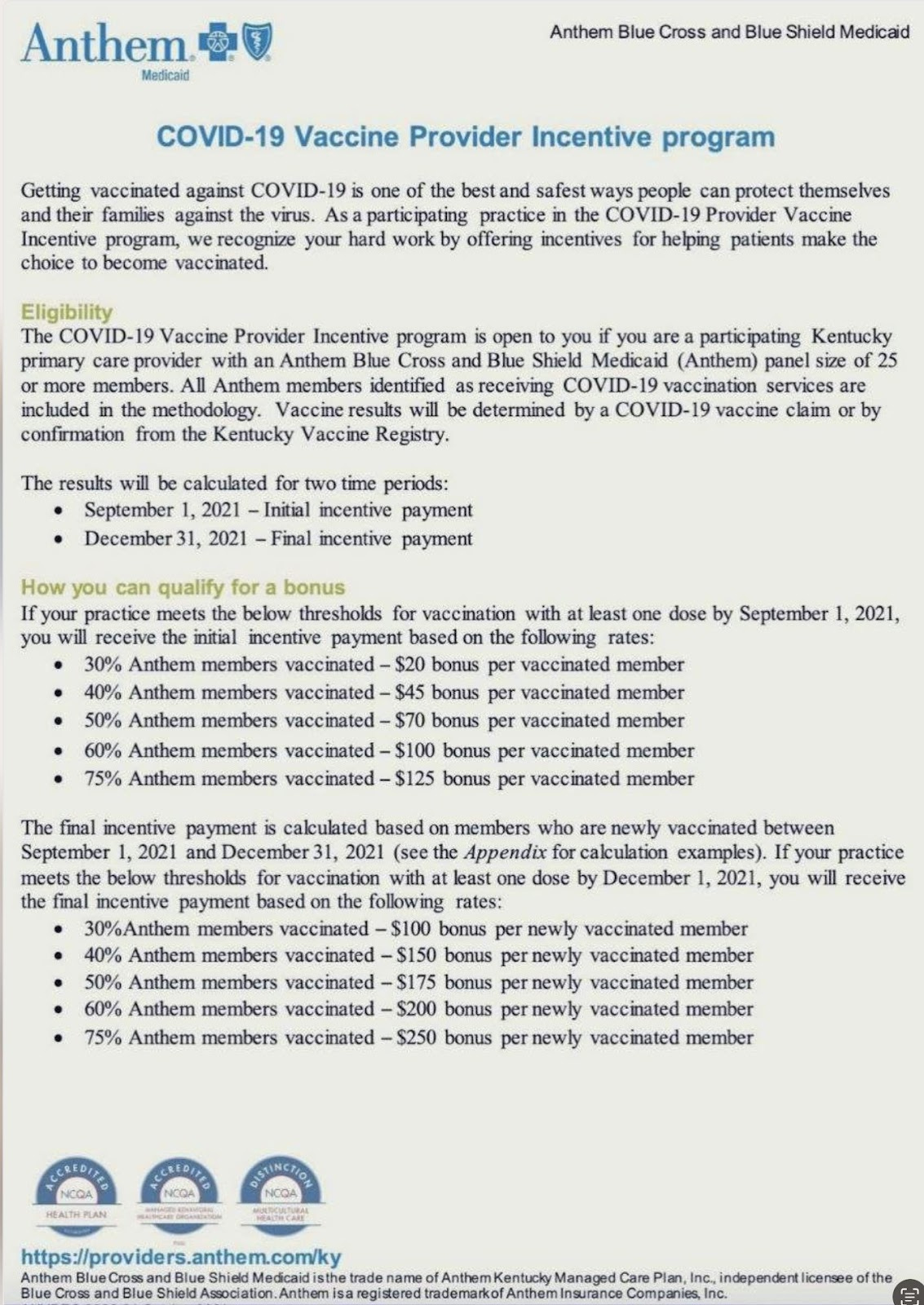
For example, Anthem Blue Cross Blue Shield (BCBS) in 2021 implemented a COVID-19 vaccine provider incentive program to boost vaccination rates by offering financial rewards to healthcare providers. Although the incentives varied by state, physicians received payments for each vaccine administered along with bonuses based on the total number of experimental COVID-19 vaccines given. This incentive structure encouraged doctors to push for higher vaccination numbers, directly impacting their overall revenue.
The program also included performance-based rewards, offering higher bonuses for practices that achieved specific vaccination targets or metrics. Enhanced reimbursement rates for vaccine administration services further contributed to the overall revenue of participating practices.
“The purpose of any performance-based incentives, where they exist, is to reward implementation of well-established, evidence-based best practices in the care of our members,” a BCBS spokesperson told USA Today in an emailed statement. “While vaccinations may fall into that category, they would not be the sole performance measure.”
It’s hard to claim bonuses were tied to a “well-established, evidenced-based best practice” when COVID-19 vaccines were entirely experimental, authorized under emergency use, and utilized a novel technology.
Moreover, young children are not an at-risk age group for COVID-19. Those who do get COVID-19 are primarily asymptomatic, rarely experience severe outcomes, and the few who do have underlying medical conditions. In fact, there are more cases of serious adverse events in kids under age five reported to the CDC’s Vaccine Adverse Event Reporting System following vaccination—which are underreported—than there are severe outcomes of COVID-19, which are overreported.
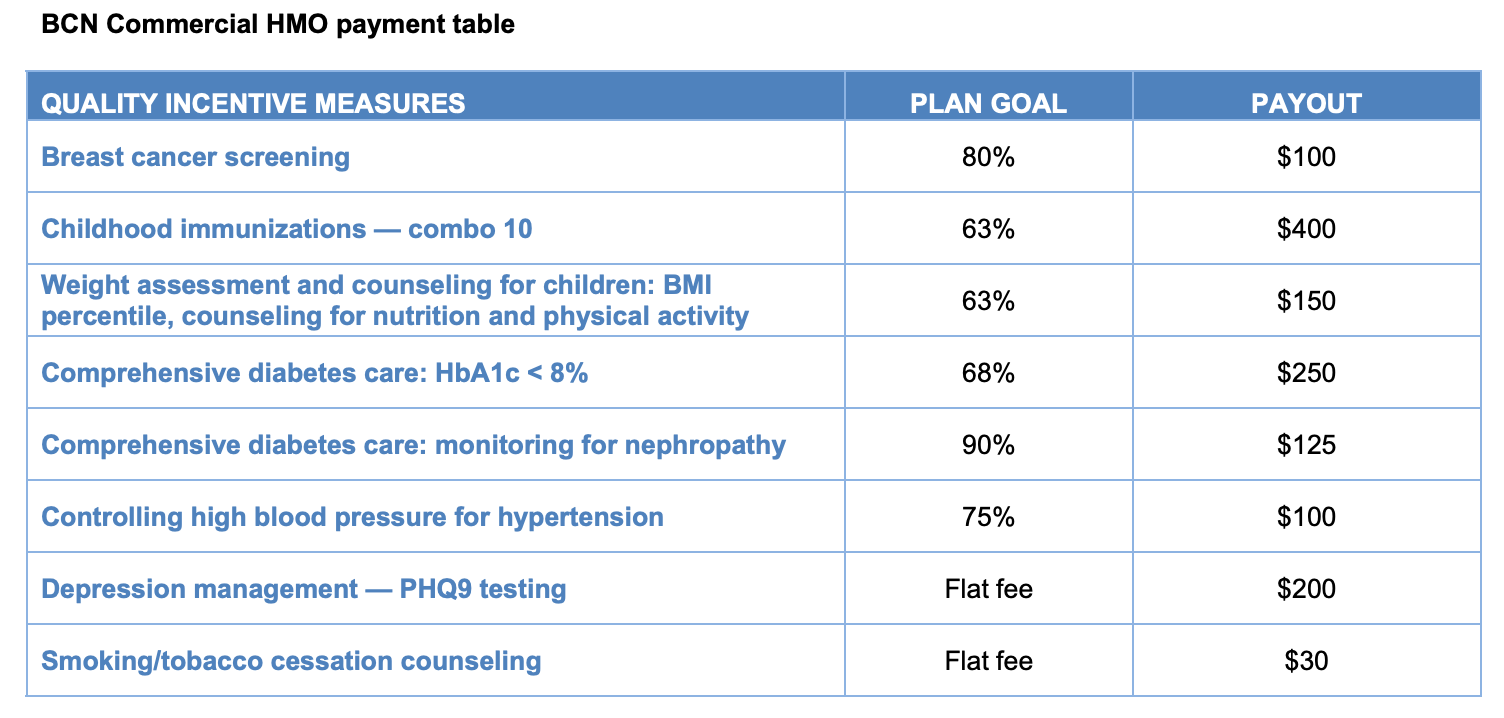
BCBS Michigan has also offered incentives to providers to vaccinate children. The company in 2016 paid pediatricians $400 for each fully vaccinated child under the age of two if at least 63% of that physician’s patient population was up-to-date on vaccinations.
Blue Cross Blue Shield Blue Care Network of Michigan told Reuters that it “periodically provides financial incentives for physicians for administering the recommended vaccines for children under the age of two.”
In a typical pediatric practice, a pediatrician might see anywhere from 100 to 200 children under age two. This number can be higher in larger practices or areas with higher birth rates. If 63% of 100 two-year-olds are fully vaccinated each year, that’s a $604,800 yearly bonus. If 100% of the physician’s two-year-old patients are fully vaccinated, that’s a $960,000 bonus.
Insurance companies also offer doctors financial incentives for cancer screenings, diabetes and high blood pressure medications, and “depression management,” which are often used to normalize vaccine incentives.
Government Sinks Billions Into Promoting COVID-19 Vaccines
In addition to the financial incentives given by the CDC and insurance companies, the federal government, through the Department of Health and Human Services, invests billions on vaccine uptake through funding that goes to pharmacies, health centers, the CDC (and then on to health departments and physician practices) and medical membership organizations like the American College of Obstetrics and Gynecology and American Academy of Pediatrics.
For example, the Biden administration in 2022 invested $350 million in community health centers and community-based organizations to “increase the pace of vaccinations.” This funding could be used for various activities, from mobile, drive-up, walk-up, or community-based vaccination events to partnerships with community and faith-based organizations for vaccination activities, raising awareness of the updated shot, and more.
The Biden administration in March 2021 made a $10 billion investment in March 2021 to expand access to vaccines and build vaccine confidence. These investments underscore the federal government’s commitment to increasing vaccination rates, but they also perpetuate a system where financial incentives play a significant role in shaping medical practices.
HHS in April 2023 created a $1.1 billion public-private partnership to help maintain uninsured individuals’ access to COVID-19 vaccines and treatments at local pharmacies. This financially incentivized pharmacies like CVS and Walgreens to vaccinate as many people as possible despite concerns and controversies surrounding the dangers of COVID-19 vaccines.
Under the program, the CDC used its existing authority to purchase and distribute COVID-19 vaccines and allocate them through its network of 64 state and local health department immunization awardees nationwide, similar to how it does with the VFC program. These awardees then distributed vaccines to participating health centers.
These examples barely scratch the surface of the vast financial interests fueling vaccine promotion. With doctors and pharmaceutical companies shielded by blanket liability protections and backed by endless government funding, there’s little incentive to acknowledge the risks of vaccines or room to allow parents to make their own informed choices.
From government programs like the VFC that reward high vaccination rates with increased funding to insurance companies offering bonuses for reaching vaccination targets, the scheme reeks of a profit-driven agenda.
This financial motivation masks itself as public health advocacy, but it is clear that the primary driver behind these policies is not the well-being of children but the financial gains of those involved in the vaccination industry.
| |||||
| |||||
Exposing and removing Big Pharma corruption. Restoring healthcare integrity. |