Email
The Connection: Increasing Coverage Through “Easy Enrollment”; New Medicaid/CHIP Rules to Improve Quality and Equity; Supporting Informal Caregivers; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Increasing Coverage Through “Easy Enrollment”; New Medicaid/CHIP Rules to Improve Quality and Equity; Supporting Informal Caregivers; and More |
| Date | July 1, 2024 4:28 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
July 1, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
Easy Enrollment Programs Increase Access to Affordable Coverage
An increasing number of states are experimenting with simple, low-cost ways to connect uninsured people with comprehensive, affordable coverage options. On To the Point, Georgetown University researchers describe how these “easy enrollment” programs combine tax or unemployment filing forms with targeted outreach to identify people who may be eligible for subsidized marketplace plans or Medicaid. The results have been promising: Maryland, the first state to enact such a program, has enrolled more than 13,500 people since 2020.
READ MORE ([link removed] )
Unlocking Better Care Quality and Access in Medicaid and CHIP
New rules from the Centers for Medicare and Medicaid Services (CMS) could improve access to care for millions covered by Medicaid and the Children’s Health Insurance Program. Manatt Health’s Cindy Mann and colleagues explain how these rules align with key CMS goals, including data transparency, new opportunities for consumer input, greater health equity, and standardization across federally funded health programs.
READ MORE ([link removed] )
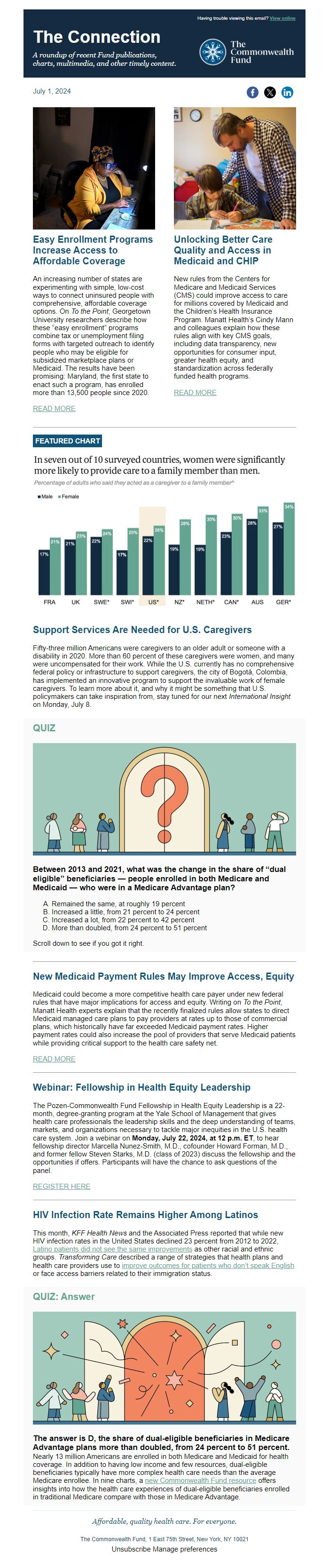
FEATURED CHART
Support Services Are Needed for U.S. Caregivers
Fifty-three million Americans were caregivers to an older adult or someone with a disability in 2020. More than 60 percent of these caregivers were women, and many were uncompensated for their work. While the U.S. currently has no comprehensive federal policy or infrastructure to support caregivers, the city of Bogotá, Colombia, has implemented an innovative program to support the invaluable work of female caregivers. To learn more about it, and why it might be something that U.S. policymakers can take inspiration from, stay tuned for our next International Insight on Monday, July 8.
QUIZ
Between 2013 and 2021, what was the change in the share of “dual eligible” beneficiaries — people enrolled in both Medicare and Medicaid — who were in a Medicare Advantage plan?
- Remained the same, at roughly 19 percent
- Increased a little, from 21 percent to 24 percent
- Increased a lot, from 22 percent to 42 percent
- More than doubled, from 24 percent to 51 percent
Scroll down to see if you got it right.
New Medicaid Payment Rules May Improve Access, Equity
Medicaid could become a more competitive health care payer under new federal rules that have major implications for access and equity. Writing on To the Point, Manatt Health experts explain that the recently finalized rules allow states to direct Medicaid managed care plans to pay providers at rates up to those of commercial plans, which historically have far exceeded Medicaid payment rates. Higher payment rates could also increase the pool of providers that serve Medicaid patients while providing critical support to the health care safety net.
READ MORE ([link removed] )
Webinar: Fellowship in Health Equity Leadership
The Pozen-Commonwealth Fund Fellowship in Health Equity Leadership is a 22-month, degree-granting program at the Yale School of Management that gives health care professionals the leadership skills and the deep understanding of teams, markets, and organizations necessary to tackle major inequities in the U.S. health care system. Join a webinar on Monday, July 22, 2024, at 12 p.m. ET, to hear fellowship director Marcella Nunez-Smith, M.D., cofounder Howard Forman, M.D., and former fellow Steven Starks, M.D. (class of 2023) discuss the fellowship and the opportunities if offers. Participants will have the chance to ask questions of the panel.
REGISTER HERE ([link removed] )
HIV Infection Rate Remains Higher Among Latinos
This month, KFF Health News and the Associated Press reported that while new HIV infection rates in the United States declined 23 percent from 2012 to 2022, Latino patients did not see the same improvements ([link removed] ) as other racial and ethnic groups. Transforming Care described a range of strategies that health plans and health care providers use to improve outcomes for patients who don’t speak English ([link removed] ) or face access barriers related to their immigration status.
QUIZ: Answer
The answer is D, the share of dual-eligible beneficiaries in Medicare Advantage plans more than doubled, from 24 percent to 51 percent.
Nearly 13 million Americans are enrolled in both Medicare and Medicaid for health coverage. In addition to having low income and few resources, dual-eligible beneficiaries typically have more complex health care needs than the average Medicare enrollee. In nine charts, a new Commonwealth Fund resource ([link removed] ) offers insights into how the health care experiences of dual-eligible beneficiaries enrolled in traditional Medicare compare with those in Medicare Advantage.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
July 1, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
Easy Enrollment Programs Increase Access to Affordable Coverage
An increasing number of states are experimenting with simple, low-cost ways to connect uninsured people with comprehensive, affordable coverage options. On To the Point, Georgetown University researchers describe how these “easy enrollment” programs combine tax or unemployment filing forms with targeted outreach to identify people who may be eligible for subsidized marketplace plans or Medicaid. The results have been promising: Maryland, the first state to enact such a program, has enrolled more than 13,500 people since 2020.
READ MORE ([link removed] )
Unlocking Better Care Quality and Access in Medicaid and CHIP
New rules from the Centers for Medicare and Medicaid Services (CMS) could improve access to care for millions covered by Medicaid and the Children’s Health Insurance Program. Manatt Health’s Cindy Mann and colleagues explain how these rules align with key CMS goals, including data transparency, new opportunities for consumer input, greater health equity, and standardization across federally funded health programs.
READ MORE ([link removed] )
FEATURED CHART
Support Services Are Needed for U.S. Caregivers
Fifty-three million Americans were caregivers to an older adult or someone with a disability in 2020. More than 60 percent of these caregivers were women, and many were uncompensated for their work. While the U.S. currently has no comprehensive federal policy or infrastructure to support caregivers, the city of Bogotá, Colombia, has implemented an innovative program to support the invaluable work of female caregivers. To learn more about it, and why it might be something that U.S. policymakers can take inspiration from, stay tuned for our next International Insight on Monday, July 8.
QUIZ
Between 2013 and 2021, what was the change in the share of “dual eligible” beneficiaries — people enrolled in both Medicare and Medicaid — who were in a Medicare Advantage plan?
- Remained the same, at roughly 19 percent
- Increased a little, from 21 percent to 24 percent
- Increased a lot, from 22 percent to 42 percent
- More than doubled, from 24 percent to 51 percent
Scroll down to see if you got it right.
New Medicaid Payment Rules May Improve Access, Equity
Medicaid could become a more competitive health care payer under new federal rules that have major implications for access and equity. Writing on To the Point, Manatt Health experts explain that the recently finalized rules allow states to direct Medicaid managed care plans to pay providers at rates up to those of commercial plans, which historically have far exceeded Medicaid payment rates. Higher payment rates could also increase the pool of providers that serve Medicaid patients while providing critical support to the health care safety net.
READ MORE ([link removed] )
Webinar: Fellowship in Health Equity Leadership
The Pozen-Commonwealth Fund Fellowship in Health Equity Leadership is a 22-month, degree-granting program at the Yale School of Management that gives health care professionals the leadership skills and the deep understanding of teams, markets, and organizations necessary to tackle major inequities in the U.S. health care system. Join a webinar on Monday, July 22, 2024, at 12 p.m. ET, to hear fellowship director Marcella Nunez-Smith, M.D., cofounder Howard Forman, M.D., and former fellow Steven Starks, M.D. (class of 2023) discuss the fellowship and the opportunities if offers. Participants will have the chance to ask questions of the panel.
REGISTER HERE ([link removed] )
HIV Infection Rate Remains Higher Among Latinos
This month, KFF Health News and the Associated Press reported that while new HIV infection rates in the United States declined 23 percent from 2012 to 2022, Latino patients did not see the same improvements ([link removed] ) as other racial and ethnic groups. Transforming Care described a range of strategies that health plans and health care providers use to improve outcomes for patients who don’t speak English ([link removed] ) or face access barriers related to their immigration status.
QUIZ: Answer
The answer is D, the share of dual-eligible beneficiaries in Medicare Advantage plans more than doubled, from 24 percent to 51 percent.
Nearly 13 million Americans are enrolled in both Medicare and Medicaid for health coverage. In addition to having low income and few resources, dual-eligible beneficiaries typically have more complex health care needs than the average Medicare enrollee. In nine charts, a new Commonwealth Fund resource ([link removed] ) offers insights into how the health care experiences of dual-eligible beneficiaries enrolled in traditional Medicare compare with those in Medicare Advantage.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
