Email
The Connection: Racial Disparities in Health Across U.S.; Access to Mental Health Care in School; Effects of Medicaid Unwinding; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Racial Disparities in Health Across U.S.; Access to Mental Health Care in School; Effects of Medicaid Unwinding; and More |
| Date | April 22, 2024 5:08 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
April 22, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
Stark Racial Disparities in Health Persist Across States
Deep-seated racial disparities in health care access, quality, and outcomes persist across all U.S. states, according to a Commonwealth Fund evaluation of 25 measures of health care access, quality, service use, and health outcomes for five racial and ethnic groups. The report shows the health care divide is especially stark when it comes to premature deaths: American Indian and Black people die from preventable and treatable causes at substantially higher rates than other groups. It also shows disparities exist even in states where the health system is otherwise high performing.
READ MORE ([link removed] )
Medicaid Can Help Students Get Mental Health Care at School
Seven of 10 schools in the United States report an increase in the number of students seeking mental health services since 2020. With growing demand for treatment, schools need additional resources to meet their needs. On To the Point, Laura Conrad and colleagues discuss the benefits of school-based mental health programs and how schools can access Medicaid funding. States can support effective and equitable school-based programming, they say, by targeting funding and assistance to small districts, providing peer-to-peer learning opportunities, and making impact data available to the public.
READ MORE ([link removed] )
FEATURED CHART
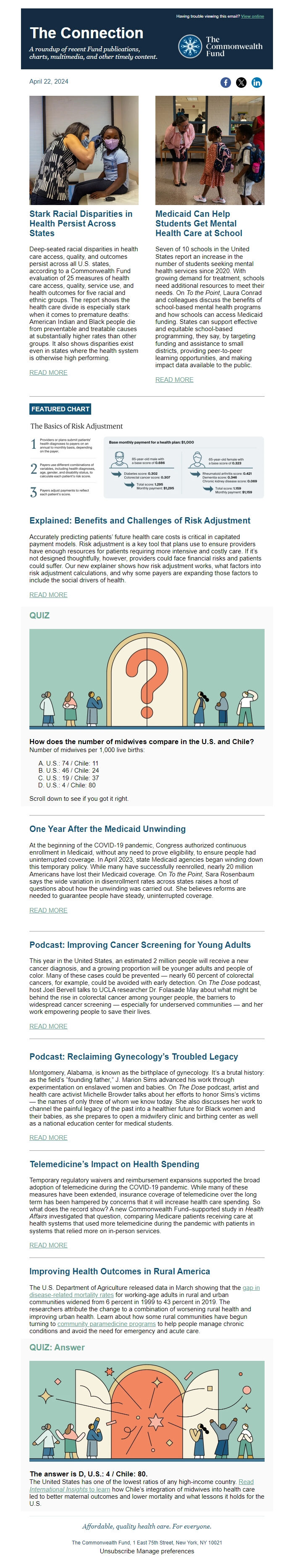
Explained: Benefits and Challenges of Risk Adjustment
Accurately predicting patients’ future health care costs is critical in capitated payment models. Risk adjustment is a key tool that plans use to ensure providers have enough resources for patients requiring more intensive and costly care. If it’s not designed thoughtfully, however, providers could face financial risks and patients could suffer. Our new explainer shows how risk adjustment works, what factors into risk adjustment calculations, and why some payers are expanding those factors to include the social drivers of health.
READ MORE ([link removed] )
QUIZ
How does the number of midwives compare in the U.S. and Chile?
Number of midwives per 1,000 live births:
- U.S.: 74 / Chile: 11
- U.S.: 46 / Chile: 24
- U.S.: 19 / Chile: 37
- U.S.: 4 / Chile: 80
Scroll down to see if you got it right.
One Year After the Medicaid Unwinding
At the beginning of the COVID-19 pandemic, Congress authorized continuous enrollment in Medicaid, without any need to prove eligibility, to ensure people had uninterrupted coverage. In April 2023, state Medicaid agencies began winding down this temporary policy. While many have successfully reenrolled, nearly 20 million Americans have lost their Medicaid coverage. On To the Point, Sara Rosenbaum says the wide variation in disenrollment rates across states raises a host of questions about how the unwinding was carried out. She believes reforms are needed to guarantee people have steady, uninterrupted coverage.
READ MORE ([link removed] )
Podcast: Improving Cancer Screening for Young Adults
This year in the United States, an estimated 2 million people will receive a new cancer diagnosis, and a growing proportion will be younger adults and people of color. Many of these cases could be prevented — nearly 60 percent of colorectal cancers, for example, could be avoided with early detection. On The Dose podcast, host Joel Bervell talks to UCLA researcher Dr. Folasade May about what might be behind the rise in colorectal cancer among younger people, the barriers to widespread cancer screening — especially for underserved communities — and her work empowering people to save their lives.
READ MORE ([link removed] )
Podcast: Reclaiming Gynecology’s Troubled Legacy
Montgomery, Alabama, is known as the birthplace of gynecology. It’s a brutal history: as the field’s “founding father,” J. Marion Sims advanced his work through experimentation on enslaved women and babies. On The Dose podcast, artist and health care activist Michelle Browder talks about her efforts to honor Sims’s victims — the names of only three of whom we know today. She also discusses her work to channel the painful legacy of the past into a healthier future for Black women and their babies, as she prepares to open a midwifery clinic and birthing center as well as a national education center for medical students.
READ MORE ([link removed] )
Telemedicine’s Impact on Health Spending
Temporary regulatory waivers and reimbursement expansions supported the broad adoption of telemedicine during the COVID-19 pandemic. While many of these measures have been extended, insurance coverage of telemedicine over the long term has been hampered by concerns that it will increase health care spending. So what does the record show? A new Commonwealth Fund–supported study in Health Affairs investigated that question, comparing Medicare patients receiving care at health systems that used more telemedicine during the pandemic with patients in systems that relied more on in-person services.
READ MORE ([link removed] )
Improving Health Outcomes in Rural America
The U.S. Department of Agriculture released data in March showing that the gap in disease-related mortality rates ([link removed] ) for working-age adults in rural and urban communities widened from 6 percent in 1999 to 43 percent in 2019. The researchers attribute the change to a combination of worsening rural health and improving urban health. Learn about how some rural communities have begun turning to community paramedicine programs ([link removed] ) to help people manage chronic conditions and avoid the need for emergency and acute care.
QUIZ: Answer
The answer is D, U.S.: 4 / Chile: 80.
The United States has one of the lowest ratios of any high-income country. Read International Insights to learn ([link removed] ) how Chile’s integration of midwives into health care led to better maternal outcomes and lower mortality and what lessons it holds for the U.S.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
April 22, 2024
Facebook ([link removed] )
X ([link removed] )
LinkedIn ([link removed] )
Stark Racial Disparities in Health Persist Across States
Deep-seated racial disparities in health care access, quality, and outcomes persist across all U.S. states, according to a Commonwealth Fund evaluation of 25 measures of health care access, quality, service use, and health outcomes for five racial and ethnic groups. The report shows the health care divide is especially stark when it comes to premature deaths: American Indian and Black people die from preventable and treatable causes at substantially higher rates than other groups. It also shows disparities exist even in states where the health system is otherwise high performing.
READ MORE ([link removed] )
Medicaid Can Help Students Get Mental Health Care at School
Seven of 10 schools in the United States report an increase in the number of students seeking mental health services since 2020. With growing demand for treatment, schools need additional resources to meet their needs. On To the Point, Laura Conrad and colleagues discuss the benefits of school-based mental health programs and how schools can access Medicaid funding. States can support effective and equitable school-based programming, they say, by targeting funding and assistance to small districts, providing peer-to-peer learning opportunities, and making impact data available to the public.
READ MORE ([link removed] )
FEATURED CHART
Explained: Benefits and Challenges of Risk Adjustment
Accurately predicting patients’ future health care costs is critical in capitated payment models. Risk adjustment is a key tool that plans use to ensure providers have enough resources for patients requiring more intensive and costly care. If it’s not designed thoughtfully, however, providers could face financial risks and patients could suffer. Our new explainer shows how risk adjustment works, what factors into risk adjustment calculations, and why some payers are expanding those factors to include the social drivers of health.
READ MORE ([link removed] )
QUIZ
How does the number of midwives compare in the U.S. and Chile?
Number of midwives per 1,000 live births:
- U.S.: 74 / Chile: 11
- U.S.: 46 / Chile: 24
- U.S.: 19 / Chile: 37
- U.S.: 4 / Chile: 80
Scroll down to see if you got it right.
One Year After the Medicaid Unwinding
At the beginning of the COVID-19 pandemic, Congress authorized continuous enrollment in Medicaid, without any need to prove eligibility, to ensure people had uninterrupted coverage. In April 2023, state Medicaid agencies began winding down this temporary policy. While many have successfully reenrolled, nearly 20 million Americans have lost their Medicaid coverage. On To the Point, Sara Rosenbaum says the wide variation in disenrollment rates across states raises a host of questions about how the unwinding was carried out. She believes reforms are needed to guarantee people have steady, uninterrupted coverage.
READ MORE ([link removed] )
Podcast: Improving Cancer Screening for Young Adults
This year in the United States, an estimated 2 million people will receive a new cancer diagnosis, and a growing proportion will be younger adults and people of color. Many of these cases could be prevented — nearly 60 percent of colorectal cancers, for example, could be avoided with early detection. On The Dose podcast, host Joel Bervell talks to UCLA researcher Dr. Folasade May about what might be behind the rise in colorectal cancer among younger people, the barriers to widespread cancer screening — especially for underserved communities — and her work empowering people to save their lives.
READ MORE ([link removed] )
Podcast: Reclaiming Gynecology’s Troubled Legacy
Montgomery, Alabama, is known as the birthplace of gynecology. It’s a brutal history: as the field’s “founding father,” J. Marion Sims advanced his work through experimentation on enslaved women and babies. On The Dose podcast, artist and health care activist Michelle Browder talks about her efforts to honor Sims’s victims — the names of only three of whom we know today. She also discusses her work to channel the painful legacy of the past into a healthier future for Black women and their babies, as she prepares to open a midwifery clinic and birthing center as well as a national education center for medical students.
READ MORE ([link removed] )
Telemedicine’s Impact on Health Spending
Temporary regulatory waivers and reimbursement expansions supported the broad adoption of telemedicine during the COVID-19 pandemic. While many of these measures have been extended, insurance coverage of telemedicine over the long term has been hampered by concerns that it will increase health care spending. So what does the record show? A new Commonwealth Fund–supported study in Health Affairs investigated that question, comparing Medicare patients receiving care at health systems that used more telemedicine during the pandemic with patients in systems that relied more on in-person services.
READ MORE ([link removed] )
Improving Health Outcomes in Rural America
The U.S. Department of Agriculture released data in March showing that the gap in disease-related mortality rates ([link removed] ) for working-age adults in rural and urban communities widened from 6 percent in 1999 to 43 percent in 2019. The researchers attribute the change to a combination of worsening rural health and improving urban health. Learn about how some rural communities have begun turning to community paramedicine programs ([link removed] ) to help people manage chronic conditions and avoid the need for emergency and acute care.
QUIZ: Answer
The answer is D, U.S.: 4 / Chile: 80.
The United States has one of the lowest ratios of any high-income country. Read International Insights to learn ([link removed] ) how Chile’s integration of midwives into health care led to better maternal outcomes and lower mortality and what lessons it holds for the U.S.
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
