| From | Nurses' Campaign To Win Medicare For All <[email protected]> |
| Subject | Black people faced the brunt of the Covid-19 pandemic |
| Date | February 15, 2024 5:44 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
[1]NNU - Medicare for All!
It’s Black History Month, so we’re taking the time each week this February
to focus on the racial disparities that exist in our current, broken
health care system. And nowhere were these disparities more evident than
during the Covid-19 pandemic. This week, we’re looking at the racial
differences in rates of Covid-19 infection, hospitalization, deaths, and
more in the United States.
Similar to maternal mortality (which we covered last week), Black patients
have experienced worse health outcomes in relation to Covid-19 than their
white counterparts.
While the gaps have narrowed since the pandemic began in 2019, overall,
Black people have experienced higher rates of Covid-19 infection and death
than white people.^1
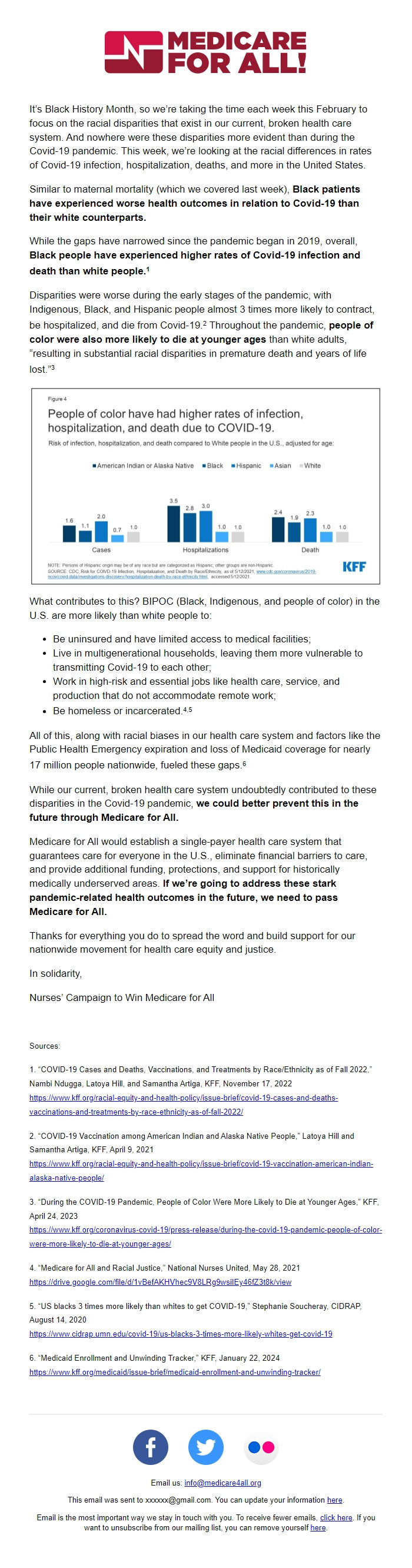
Disparities were worse during the early stages of the pandemic, with
Indigenous, Black, and Hispanic people almost 3 times more likely to
contract, be hospitalized, and die from Covid-19.^2 Throughout the
pandemic, people of color were also more likely to die at younger ages
than white adults, “resulting in substantial racial disparities in
premature death and years of life lost.”^3
[ [link removed] ]^[ [link removed] ]KFF Figure 4: People of color have had higher rates of infection,
hospitalization, and death due to COVID-19.
What contributes to this? BIPOC (Black, Indigenous, and people of color)
in the U.S. are more likely than white people to:
* Be uninsured and have limited access to medical facilities;
* Live in multigenerational households, leaving them more vulnerable to
transmitting Covid-19 to each other;
* Work in high-risk and essential jobs like health care, service, and
production that do not accommodate remote work;
* Be homeless or incarcerated.^4,5
All of this, along with racial biases in our health care system and
factors like the Public Health Emergency expiration and loss of Medicaid
coverage for nearly 17 million people nationwide, fueled these gaps.^6
While our current, broken health care system undoubtedly contributed to
these disparities in the Covid-19 pandemic, we could better prevent this
in the future through Medicare for All.
Medicare for All would establish a single-payer health care system that
guarantees care for everyone in the U.S., eliminate financial barriers to
care, and provide additional funding, protections, and support for
historically medically underserved areas. If we’re going to address these
stark pandemic-related health outcomes in the future, we need to pass
Medicare for All.
Thanks for everything you do to spread the word and build support for our
nationwide movement for health care equity and justice.
In solidarity,
Nurses’ Campaign to Win Medicare for All
Sources:
1. “COVID-19 Cases and Deaths, Vaccinations, and Treatments by
Race/Ethnicity as of Fall 2022,” Nambi Ndugga, Latoya Hill, and Samantha
Artiga, KFF, November 17, 2022
[ [link removed] ][link removed]
2. “COVID-19 Vaccination among American Indian and Alaska Native People,”
Latoya Hill and Samantha Artiga, KFF, April 9, 2021
[ [link removed] ][link removed]
3. “During the COVID-19 Pandemic, People of Color Were More Likely to Die
at Younger Ages,” KFF, April 24, 2023
[ [link removed] ][link removed]
4. “Medicare for All and Racial Justice,” National Nurses United, May 28,
2021
[ [link removed] ][link removed]
5. “US blacks 3 times more likely than whites to get COVID-19,” Stephanie
Soucheray, CIDRAP, August 14, 2020
[ [link removed] ][link removed]
6. “Medicaid Enrollment and Unwinding Tracker,” KFF, January 22, 2024
[ [link removed] ][link removed]
You can unsubscribe from this mailing list at any time:
[link removed]
It’s Black History Month, so we’re taking the time each week this February
to focus on the racial disparities that exist in our current, broken
health care system. And nowhere were these disparities more evident than
during the Covid-19 pandemic. This week, we’re looking at the racial
differences in rates of Covid-19 infection, hospitalization, deaths, and
more in the United States.
Similar to maternal mortality (which we covered last week), Black patients
have experienced worse health outcomes in relation to Covid-19 than their
white counterparts.
While the gaps have narrowed since the pandemic began in 2019, overall,
Black people have experienced higher rates of Covid-19 infection and death
than white people.^1
Disparities were worse during the early stages of the pandemic, with
Indigenous, Black, and Hispanic people almost 3 times more likely to
contract, be hospitalized, and die from Covid-19.^2 Throughout the
pandemic, people of color were also more likely to die at younger ages
than white adults, “resulting in substantial racial disparities in
premature death and years of life lost.”^3
[ [link removed] ]^[ [link removed] ]KFF Figure 4: People of color have had higher rates of infection,
hospitalization, and death due to COVID-19.
What contributes to this? BIPOC (Black, Indigenous, and people of color)
in the U.S. are more likely than white people to:
* Be uninsured and have limited access to medical facilities;
* Live in multigenerational households, leaving them more vulnerable to
transmitting Covid-19 to each other;
* Work in high-risk and essential jobs like health care, service, and
production that do not accommodate remote work;
* Be homeless or incarcerated.^4,5
All of this, along with racial biases in our health care system and
factors like the Public Health Emergency expiration and loss of Medicaid
coverage for nearly 17 million people nationwide, fueled these gaps.^6
While our current, broken health care system undoubtedly contributed to
these disparities in the Covid-19 pandemic, we could better prevent this
in the future through Medicare for All.
Medicare for All would establish a single-payer health care system that
guarantees care for everyone in the U.S., eliminate financial barriers to
care, and provide additional funding, protections, and support for
historically medically underserved areas. If we’re going to address these
stark pandemic-related health outcomes in the future, we need to pass
Medicare for All.
Thanks for everything you do to spread the word and build support for our
nationwide movement for health care equity and justice.
In solidarity,
Nurses’ Campaign to Win Medicare for All
Sources:
1. “COVID-19 Cases and Deaths, Vaccinations, and Treatments by
Race/Ethnicity as of Fall 2022,” Nambi Ndugga, Latoya Hill, and Samantha
Artiga, KFF, November 17, 2022
[ [link removed] ][link removed]
2. “COVID-19 Vaccination among American Indian and Alaska Native People,”
Latoya Hill and Samantha Artiga, KFF, April 9, 2021
[ [link removed] ][link removed]
3. “During the COVID-19 Pandemic, People of Color Were More Likely to Die
at Younger Ages,” KFF, April 24, 2023
[ [link removed] ][link removed]
4. “Medicare for All and Racial Justice,” National Nurses United, May 28,
2021
[ [link removed] ][link removed]
5. “US blacks 3 times more likely than whites to get COVID-19,” Stephanie
Soucheray, CIDRAP, August 14, 2020
[ [link removed] ][link removed]
6. “Medicaid Enrollment and Unwinding Tracker,” KFF, January 22, 2024
[ [link removed] ][link removed]
You can unsubscribe from this mailing list at any time:
[link removed]
Message Analysis
- Sender: National Nurses United
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
-
Email Providers:
- ActionKit
