Email
The Connection: Unaffordable Health Care; Medical Debt Is Making Us Sick; Toll of Unpaid Family Caregiving; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Unaffordable Health Care; Medical Debt Is Making Us Sick; Toll of Unpaid Family Caregiving; and More |
| Date | October 30, 2023 3:55 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
October 30, 2023
Facebook ([link removed] )
Twitter ([link removed] )
LinkedIn ([link removed] )
Regardless of Coverage, Many Americans Can’t Afford Their Health Care
How do health care costs affect the ability of Americans with insurance to afford health care when they need it? According to a new Commonwealth Fund survey, having insurance doesn’t guarantee access to affordable care. More than half of all working-age Americans reported they struggle with health care costs, and more than one of three are saddled with medical debt. “While having health insurance is always better than being uninsured, even people who have insurance frequently cannot afford care,” says the Fund’s Sara R. Collins.
READ MORE ([link removed] )
How Medical Debt Makes People Sicker
Nearly one in five Americans have medical debt. Black households are disproportionately affected, carrying higher amounts of debt at higher rates. On The Dose podcast, host Joel Bervell talks to Berneta Haynes of the National Consumer Law Center about the history of medical debt and discusses efforts to ease pressure on the families and communities hit hardest. Haynes describes Black Americans’ medical debt burden as a continual cycle, with many left without savings or family resources to tap into when faced with an unexpected medical bill.
READ MORE ([link removed] )
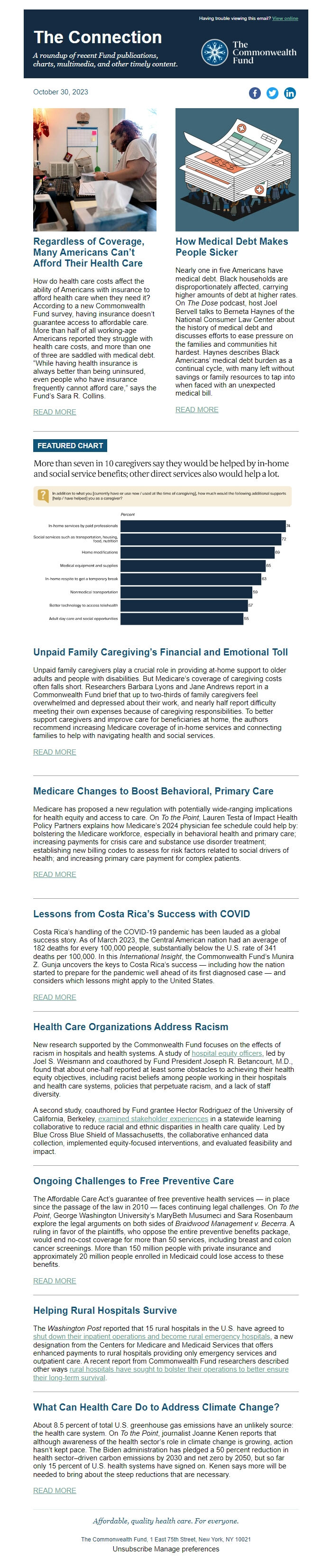
FEATURED CHART
Unpaid Family Caregiving’s Financial and Emotional Toll
Unpaid family caregivers play a crucial role in providing at-home support to older adults and people with disabilities. But Medicare’s coverage of caregiving costs often falls short. Researchers Barbara Lyons and Jane Andrews report in a Commonwealth Fund brief that up to two-thirds of family caregivers feel overwhelmed and depressed about their work, and nearly half report difficulty meeting their own expenses because of caregiving responsibilities. To better support caregivers and improve care for beneficiaries at home, the authors recommend increasing Medicare coverage of in-home services and connecting families to help with navigating health and social services.
READ MORE ([link removed] )
Medicare Changes to Boost Behavioral, Primary Care
Medicare has proposed a new regulation with potentially wide-ranging implications for health equity and access to care. On To the Point, Lauren Testa of Impact Health Policy Partners explains how Medicare’s 2024 physician fee schedule could help by: bolstering the Medicare workforce, especially in behavioral health and primary care; increasing payments for crisis care and substance use disorder treatment; establishing new billing codes to assess for risk factors related to social drivers of health; and increasing primary care payment for complex patients.
READ MORE ([link removed] )
Lessons from Costa Rica’s Success with COVID
Costa Rica’s handling of the COVID-19 pandemic has been lauded as a global success story. As of March 2023, the Central American nation had an average of 182 deaths for every 100,000 people, substantially below the U.S. rate of 341 deaths per 100,000. In this International Insight, the Commonwealth Fund’s Munira Z. Gunja uncovers the keys to Costa Rica’s success — including how the nation started to prepare for the pandemic well ahead of its first diagnosed case — and considers which lessons might apply to the United States.
READ MORE ([link removed] )
Health Care Organizations Address Racism
New research supported by the Commonwealth Fund focuses on the effects of racism in hospitals and health systems. A study of hospital equity officers ([link removed] ) , led by Joel S. Weismann and coauthored by Fund President Joseph R. Betancourt, M.D., found that about one-half reported at least some obstacles to achieving their health equity objectives, including racist beliefs among people working in their hospitals and health care systems, policies that perpetuate racism, and a lack of staff diversity.
A second study, coauthored by Fund grantee Hector Rodriguez of the University of California, Berkeley, examined stakeholder experiences ([link removed] ) in a statewide learning collaborative to reduce racial and ethnic disparities in health care quality. Led by Blue Cross Blue Shield of Massachusetts, the collaborative enhanced data collection, implemented equity-focused interventions, and evaluated feasibility and impact.
Ongoing Challenges to Free Preventive Care
The Affordable Care Act’s guarantee of free preventive health services — in place since the passage of the law in 2010 — faces continuing legal challenges. On To the Point, George Washington University’s MaryBeth Musumeci and Sara Rosenbaum explore the legal arguments on both sides of Braidwood Management v. Becerra. A ruling in favor of the plaintiffs, who oppose the entire preventive benefits package, would end no-cost coverage for more than 50 services, including breast and colon cancer screenings. More than 150 million people with private insurance and approximately 20 million people enrolled in Medicaid could lose access to these benefits.
READ MORE ([link removed] )
Helping Rural Hospitals Survive
The Washington Post reported that 15 rural hospitals in the U.S. have agreed to shut down their inpatient operations and become rural emergency hospitals ([link removed] ) , a new designation from the Centers for Medicare and Medicaid Services that offers enhanced payments to rural hospitals providing only emergency services and outpatient care. A recent report from Commonwealth Fund researchers described other ways rural hospitals have sought to bolster their operations to better ensure their long-term survival ([link removed] ) .
What Can Health Care Do to Address Climate Change?
About 8.5 percent of total U.S. greenhouse gas emissions have an unlikely source: the health care system. On To the Point, journalist Joanne Kenen reports that although awareness of the health sector’s role in climate change is growing, action hasn’t kept pace. The Biden administration has pledged a 50 percent reduction in health sector–driven carbon emissions by 2030 and net zero by 2050, but so far only 15 percent of U.S. health systems have signed on. Kenen says more will be needed to bring about the steep reductions that are necessary.
READ MORE ([link removed] )
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
October 30, 2023
Facebook ([link removed] )
Twitter ([link removed] )
LinkedIn ([link removed] )
Regardless of Coverage, Many Americans Can’t Afford Their Health Care
How do health care costs affect the ability of Americans with insurance to afford health care when they need it? According to a new Commonwealth Fund survey, having insurance doesn’t guarantee access to affordable care. More than half of all working-age Americans reported they struggle with health care costs, and more than one of three are saddled with medical debt. “While having health insurance is always better than being uninsured, even people who have insurance frequently cannot afford care,” says the Fund’s Sara R. Collins.
READ MORE ([link removed] )
How Medical Debt Makes People Sicker
Nearly one in five Americans have medical debt. Black households are disproportionately affected, carrying higher amounts of debt at higher rates. On The Dose podcast, host Joel Bervell talks to Berneta Haynes of the National Consumer Law Center about the history of medical debt and discusses efforts to ease pressure on the families and communities hit hardest. Haynes describes Black Americans’ medical debt burden as a continual cycle, with many left without savings or family resources to tap into when faced with an unexpected medical bill.
READ MORE ([link removed] )
FEATURED CHART
Unpaid Family Caregiving’s Financial and Emotional Toll
Unpaid family caregivers play a crucial role in providing at-home support to older adults and people with disabilities. But Medicare’s coverage of caregiving costs often falls short. Researchers Barbara Lyons and Jane Andrews report in a Commonwealth Fund brief that up to two-thirds of family caregivers feel overwhelmed and depressed about their work, and nearly half report difficulty meeting their own expenses because of caregiving responsibilities. To better support caregivers and improve care for beneficiaries at home, the authors recommend increasing Medicare coverage of in-home services and connecting families to help with navigating health and social services.
READ MORE ([link removed] )
Medicare Changes to Boost Behavioral, Primary Care
Medicare has proposed a new regulation with potentially wide-ranging implications for health equity and access to care. On To the Point, Lauren Testa of Impact Health Policy Partners explains how Medicare’s 2024 physician fee schedule could help by: bolstering the Medicare workforce, especially in behavioral health and primary care; increasing payments for crisis care and substance use disorder treatment; establishing new billing codes to assess for risk factors related to social drivers of health; and increasing primary care payment for complex patients.
READ MORE ([link removed] )
Lessons from Costa Rica’s Success with COVID
Costa Rica’s handling of the COVID-19 pandemic has been lauded as a global success story. As of March 2023, the Central American nation had an average of 182 deaths for every 100,000 people, substantially below the U.S. rate of 341 deaths per 100,000. In this International Insight, the Commonwealth Fund’s Munira Z. Gunja uncovers the keys to Costa Rica’s success — including how the nation started to prepare for the pandemic well ahead of its first diagnosed case — and considers which lessons might apply to the United States.
READ MORE ([link removed] )
Health Care Organizations Address Racism
New research supported by the Commonwealth Fund focuses on the effects of racism in hospitals and health systems. A study of hospital equity officers ([link removed] ) , led by Joel S. Weismann and coauthored by Fund President Joseph R. Betancourt, M.D., found that about one-half reported at least some obstacles to achieving their health equity objectives, including racist beliefs among people working in their hospitals and health care systems, policies that perpetuate racism, and a lack of staff diversity.
A second study, coauthored by Fund grantee Hector Rodriguez of the University of California, Berkeley, examined stakeholder experiences ([link removed] ) in a statewide learning collaborative to reduce racial and ethnic disparities in health care quality. Led by Blue Cross Blue Shield of Massachusetts, the collaborative enhanced data collection, implemented equity-focused interventions, and evaluated feasibility and impact.
Ongoing Challenges to Free Preventive Care
The Affordable Care Act’s guarantee of free preventive health services — in place since the passage of the law in 2010 — faces continuing legal challenges. On To the Point, George Washington University’s MaryBeth Musumeci and Sara Rosenbaum explore the legal arguments on both sides of Braidwood Management v. Becerra. A ruling in favor of the plaintiffs, who oppose the entire preventive benefits package, would end no-cost coverage for more than 50 services, including breast and colon cancer screenings. More than 150 million people with private insurance and approximately 20 million people enrolled in Medicaid could lose access to these benefits.
READ MORE ([link removed] )
Helping Rural Hospitals Survive
The Washington Post reported that 15 rural hospitals in the U.S. have agreed to shut down their inpatient operations and become rural emergency hospitals ([link removed] ) , a new designation from the Centers for Medicare and Medicaid Services that offers enhanced payments to rural hospitals providing only emergency services and outpatient care. A recent report from Commonwealth Fund researchers described other ways rural hospitals have sought to bolster their operations to better ensure their long-term survival ([link removed] ) .
What Can Health Care Do to Address Climate Change?
About 8.5 percent of total U.S. greenhouse gas emissions have an unlikely source: the health care system. On To the Point, journalist Joanne Kenen reports that although awareness of the health sector’s role in climate change is growing, action hasn’t kept pace. The Biden administration has pledged a 50 percent reduction in health sector–driven carbon emissions by 2030 and net zero by 2050, but so far only 15 percent of U.S. health systems have signed on. Kenen says more will be needed to bring about the steep reductions that are necessary.
READ MORE ([link removed] )
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
-
Email Providers:
- HubSpot
