Email
The Connection: Older Adults with Employer Coverage; Value-Based Payment and Health Equity; Dissatisfied Primary Care Physicians; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Older Adults with Employer Coverage; Value-Based Payment and Health Equity; Dissatisfied Primary Care Physicians; and More |
| Date | August 21, 2023 5:54 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
August 21, 2023
Facebook ([link removed] )
Twitter ([link removed] )
LinkedIn ([link removed] )
Many Older Adults in Employer Plans Can’t Afford Care
With premiums and deductibles outpacing income growth over the past decade, employer health plans are failing to protect many older adults from health costs or ensure access to affordable care, a new Commonwealth Fund study shows. Large shares of adults ages 50 to 64 in these plans, especially people with low or moderate income, can’t afford needed care and struggle to pay their medical bills. Learn what policymakers can do to expand coverage options for people in this age group.
READ MORE ([link removed] )
Changing How We Pay for Care Can Promote Health Equity
Inequities in health and health care are pervasive and persistent in the United States, in part due to discrimination inside and outside our health care system. One way to increase health equity is reforming how we pay for care, says the Commonwealth Fund’s Celli Horstman. She makes the case for replacing the prevailing fee-for-service model in U.S. health care — designed primarily to address sickness — with an advanced value-based payment system that promotes long-term health and well-being.
READ MORE ([link removed] )
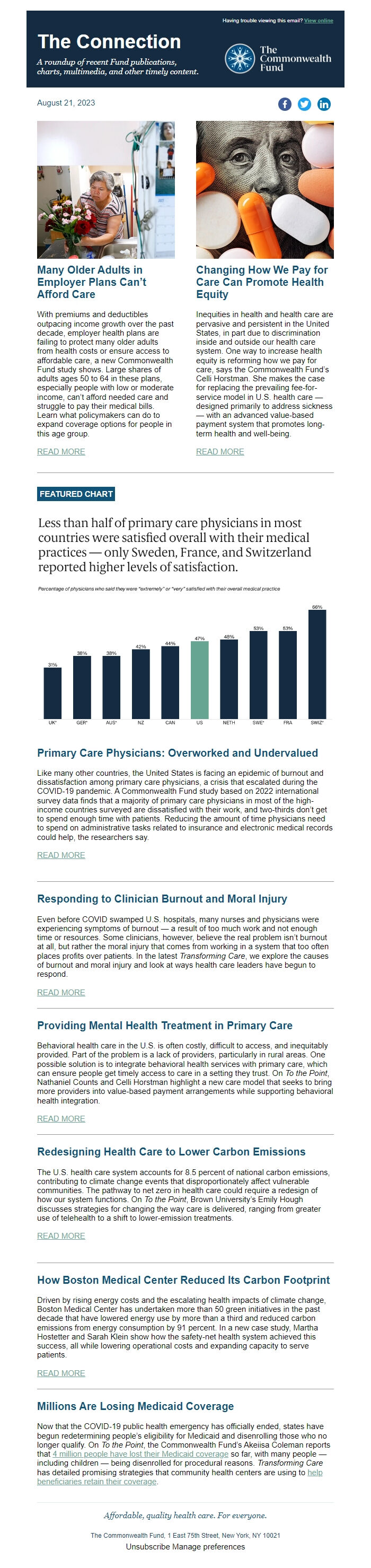
FEATURED CHART
Primary Care Physicians: Overworked and Undervalued
Like many other countries, the United States is facing an epidemic of burnout and dissatisfaction among primary care physicians, a crisis that escalated during the COVID-19 pandemic. A Commonwealth Fund study based on 2022 international survey data finds that a majority of primary care physicians in most of the high-income countries surveyed are dissatisfied with their work, and two-thirds don’t get to spend enough time with patients. Reducing the amount of time physicians need to spend on administrative tasks related to insurance and electronic medical records could help, the researchers say.
READ MORE ([link removed] )
Responding to Clinician Burnout and Moral Injury
Even before COVID swamped U.S. hospitals, many nurses and physicians were experiencing symptoms of burnout — a result of too much work and not enough time or resources. Some clinicians, however, believe the real problem isn’t burnout at all, but rather the moral injury that comes from working in a system that too often places profits over patients. In the latest Transforming Care, we explore the causes of burnout and moral injury and look at ways health care leaders have begun to respond.
READ MORE ([link removed] )
Providing Mental Health Treatment in Primary Care
Behavioral health care in the U.S. is often costly, difficult to access, and inequitably provided. Part of the problem is a lack of providers, particularly in rural areas. One possible solution is to integrate behavioral health services with primary care, which can ensure people get timely access to care in a setting they trust. On To the Point, Nathaniel Counts and Celli Horstman highlight a new care model that seeks to bring more providers into value-based payment arrangements while supporting behavioral health integration.
READ MORE ([link removed] )
Redesigning Health Care to Lower Carbon Emissions
The U.S. health care system accounts for 8.5 percent of national carbon emissions, contributing to climate change events that disproportionately affect vulnerable communities. The pathway to net zero in health care could require a redesign of how our system functions. On To the Point, Brown University’s Emily Hough discusses strategies for changing the way care is delivered, ranging from greater use of telehealth to a shift to lower-emission treatments.
READ MORE ([link removed] )
How Boston Medical Center Reduced Its Carbon Footprint
Driven by rising energy costs and the escalating health impacts of climate change, Boston Medical Center has undertaken more than 50 green initiatives in the past decade that have lowered energy use by more than a third and reduced carbon emissions from energy consumption by 91 percent. In a new case study, Martha Hostetter and Sarah Klein show how the safety-net health system achieved this success, all while lowering operational costs and expanding capacity to serve patients.
READ MORE ([link removed] )
Millions Are Losing Medicaid Coverage
Now that the COVID-19 public health emergency has officially ended, states have begun redetermining people’s eligibility for Medicaid and disenrolling those who no longer qualify. On To the Point, the Commonwealth Fund’s Akeiisa Coleman reports that 4 million people have lost their Medicaid coverage ([link removed] ) so far, with many people — including children — being disenrolled for procedural reasons. Transforming Care has detailed promising strategies that community health centers are using to help beneficiaries retain their coverage ([link removed] ) .
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
August 21, 2023
Facebook ([link removed] )
Twitter ([link removed] )
LinkedIn ([link removed] )
Many Older Adults in Employer Plans Can’t Afford Care
With premiums and deductibles outpacing income growth over the past decade, employer health plans are failing to protect many older adults from health costs or ensure access to affordable care, a new Commonwealth Fund study shows. Large shares of adults ages 50 to 64 in these plans, especially people with low or moderate income, can’t afford needed care and struggle to pay their medical bills. Learn what policymakers can do to expand coverage options for people in this age group.
READ MORE ([link removed] )
Changing How We Pay for Care Can Promote Health Equity
Inequities in health and health care are pervasive and persistent in the United States, in part due to discrimination inside and outside our health care system. One way to increase health equity is reforming how we pay for care, says the Commonwealth Fund’s Celli Horstman. She makes the case for replacing the prevailing fee-for-service model in U.S. health care — designed primarily to address sickness — with an advanced value-based payment system that promotes long-term health and well-being.
READ MORE ([link removed] )
FEATURED CHART
Primary Care Physicians: Overworked and Undervalued
Like many other countries, the United States is facing an epidemic of burnout and dissatisfaction among primary care physicians, a crisis that escalated during the COVID-19 pandemic. A Commonwealth Fund study based on 2022 international survey data finds that a majority of primary care physicians in most of the high-income countries surveyed are dissatisfied with their work, and two-thirds don’t get to spend enough time with patients. Reducing the amount of time physicians need to spend on administrative tasks related to insurance and electronic medical records could help, the researchers say.
READ MORE ([link removed] )
Responding to Clinician Burnout and Moral Injury
Even before COVID swamped U.S. hospitals, many nurses and physicians were experiencing symptoms of burnout — a result of too much work and not enough time or resources. Some clinicians, however, believe the real problem isn’t burnout at all, but rather the moral injury that comes from working in a system that too often places profits over patients. In the latest Transforming Care, we explore the causes of burnout and moral injury and look at ways health care leaders have begun to respond.
READ MORE ([link removed] )
Providing Mental Health Treatment in Primary Care
Behavioral health care in the U.S. is often costly, difficult to access, and inequitably provided. Part of the problem is a lack of providers, particularly in rural areas. One possible solution is to integrate behavioral health services with primary care, which can ensure people get timely access to care in a setting they trust. On To the Point, Nathaniel Counts and Celli Horstman highlight a new care model that seeks to bring more providers into value-based payment arrangements while supporting behavioral health integration.
READ MORE ([link removed] )
Redesigning Health Care to Lower Carbon Emissions
The U.S. health care system accounts for 8.5 percent of national carbon emissions, contributing to climate change events that disproportionately affect vulnerable communities. The pathway to net zero in health care could require a redesign of how our system functions. On To the Point, Brown University’s Emily Hough discusses strategies for changing the way care is delivered, ranging from greater use of telehealth to a shift to lower-emission treatments.
READ MORE ([link removed] )
How Boston Medical Center Reduced Its Carbon Footprint
Driven by rising energy costs and the escalating health impacts of climate change, Boston Medical Center has undertaken more than 50 green initiatives in the past decade that have lowered energy use by more than a third and reduced carbon emissions from energy consumption by 91 percent. In a new case study, Martha Hostetter and Sarah Klein show how the safety-net health system achieved this success, all while lowering operational costs and expanding capacity to serve patients.
READ MORE ([link removed] )
Millions Are Losing Medicaid Coverage
Now that the COVID-19 public health emergency has officially ended, states have begun redetermining people’s eligibility for Medicaid and disenrolling those who no longer qualify. On To the Point, the Commonwealth Fund’s Akeiisa Coleman reports that 4 million people have lost their Medicaid coverage ([link removed] ) so far, with many people — including children — being disenrolled for procedural reasons. Transforming Care has detailed promising strategies that community health centers are using to help beneficiaries retain their coverage ([link removed] ) .
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
-
Email Providers:
- HubSpot
