Email
The Connection: Diversity in Medical Education; Women in Cardiology; Value-Based Payment for Drugs; and More
| From | The Commonwealth Fund <[email protected]> |
| Subject | The Connection: Diversity in Medical Education; Women in Cardiology; Value-Based Payment for Drugs; and More |
| Date | July 24, 2023 7:48 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
The Connection
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
July 24, 2023
Facebook ([link removed] )
Twitter ([link removed] )
LinkedIn ([link removed] )
The Case for Diversity in Medical Education
The Supreme Court may have struck down race-conscious affirmative action in undergraduate admissions policies, but the case for diversity in medical education and health professions training is as strong as ever, say the Commonwealth Fund’s Laurie Zephyrin, M.D., the National Health Law Program’s Josemiguel Rodriguez, and George Washington University’s Sara Rosenbaum. On To the Point, they cite the overwhelming evidence of racial and ethnic disparities in health and health care as well as research showing that a diverse health care workforce improves access and outcomes, especially for patients of color.
READ MORE ([link removed] )
We Need More Women in Cardiology. Here’s Why.
Forty-four percent of U.S. women now live with some form of heart disease. And although it’s the leading cause of death among women, just 14 percent of cardiologists are women. On The Dose podcast, Joel Bervell interviews cardiologist Martha Gulati, M.D., associate director of the Barbra Streisand Women’s Heart Center at Cedars-Sinai Heart Institute in Los Angeles. She talks about women’s historical exclusion from clinical trials for heart disease, why sex and gender matter in the search for better treatments, and the persistent gaps in women’s cardiology care and research — especially related to women of color.
LISTEN NOW ([link removed] )
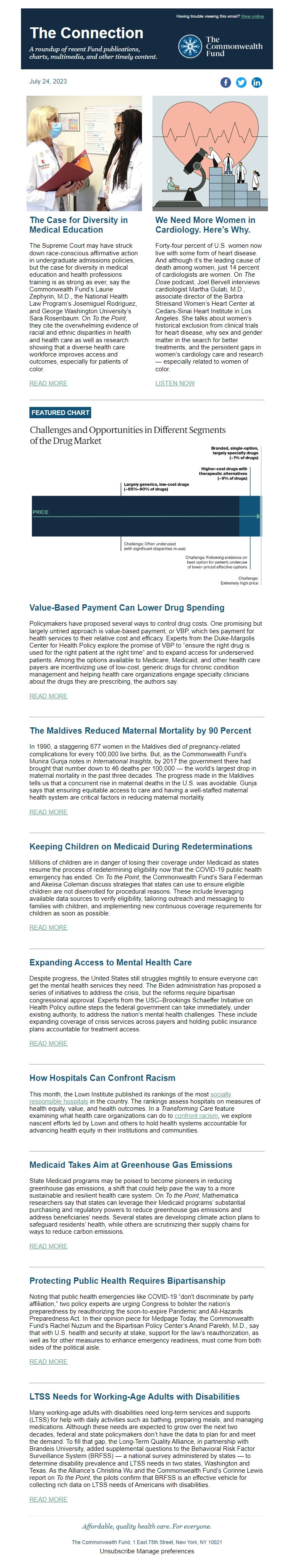
FEATURED CHART
Value-Based Payment Can Lower Drug Spending
Policymakers have proposed several ways to control drug costs. One promising but largely untried approach is value-based payment, or VBP, which ties payment for health services to their relative cost and efficacy. Experts from the Duke-Margolis Center for Health Policy explore the promise of VBP to “ensure the right drug is used for the right patient at the right time” and to expand access for underserved patients. Among the options available to Medicare, Medicaid, and other health care payers are incentivizing use of low-cost, generic drugs for chronic condition management and helping health care organizations engage specialty clinicians about the drugs they are prescribing, the authors say.
READ MORE ([link removed] )
The Maldives Reduced Maternal Mortality by 90 Percent
In 1990, a staggering 677 women in the Maldives died of pregnancy-related complications for every 100,000 live births. But, as the Commonwealth Fund’s Munira Gunja notes in International Insights, by 2017 the government there had brought that number down to 46 deaths per 100,000 — the world’s largest drop in maternal mortality in the past three decades. The progress made in the Maldives tells us that a concurrent rise in maternal deaths in the U.S. was avoidable. Gunja says that ensuring equitable access to care and having a well-staffed maternal health system are critical factors in reducing maternal mortality.
READ MORE ([link removed] )
Keeping Children on Medicaid During Redeterminations
Millions of children are in danger of losing their coverage under Medicaid as states resume the process of redetermining eligibility now that the COVID-19 public health emergency has ended. On To the Point, the Commonwealth Fund’s Sara Federman and Akeiisa Coleman discuss strategies that states can use to ensure eligible children are not disenrolled for procedural reasons. These include leveraging available data sources to verify eligibility, tailoring outreach and messaging to families with children, and implementing new continuous coverage requirements for children as soon as possible.
READ MORE ([link removed] )
Expanding Access to Mental Health Care
Despite progress, the United States still struggles mightily to ensure everyone can get the mental health services they need. The Biden administration has proposed a series of initiatives to address the crisis, but the reforms require bipartisan congressional approval. Experts from the USC–Brookings Schaeffer Initiative on Health Policy outline steps the federal government can take immediately, under existing authority, to address the nation’s mental health challenges. These include expanding coverage of crisis services across payers and holding public insurance plans accountable for treatment access.
READ MORE ([link removed] )
How Hospitals Can Confront Racism
This month, the Lown Institute published its rankings of the most socially responsible hospitals ([link removed] ) in the country. The rankings assess hospitals on measures of health equity, value, and health outcomes. In a Transforming Care feature examining what health care organizations can do to confront racism ([link removed] ) , we explore nascent efforts led by Lown and others to hold health systems accountable for advancing health equity in their institutions and communities.
Medicaid Takes Aim at Greenhouse Gas Emissions
State Medicaid programs may be poised to become pioneers in reducing greenhouse gas emissions, a shift that could help pave the way to a more sustainable and resilient health care system. On To the Point, Mathematica researchers say that states can leverage their Medicaid programs’ substantial purchasing and regulatory powers to reduce greenhouse gas emissions and address beneficiaries' needs. Several states are developing climate action plans to safeguard residents’ health, while others are scrutinizing their supply chains for ways to reduce carbon emissions.
READ MORE ([link removed] )
Protecting Public Health Requires Bipartisanship
Noting that public health emergencies like COVID-19 “don't discriminate by party affiliation,” two policy experts are urging Congress to bolster the nation’s preparedness by reauthorizing the soon-to-expire Pandemic and All-Hazards Preparedness Act. In their opinion piece for Medpage Today, the Commonwealth Fund’s Rachel Nuzum and the Bipartisan Policy Center’s Anand Parekh, M.D., say that with U.S. health and security at stake, support for the law’s reauthorization, as well as for other measures to enhance emergency readiness, must come from both sides of the political aisle.
READ MORE ([link removed] )
LTSS Needs for Working-Age Adults with Disabilities
Many working-age adults with disabilities need long-term services and supports (LTSS) for help with daily activities such as bathing, preparing meals, and managing medications. Although these needs are expected to grow over the next two decades, federal and state policymakers don’t have the data to plan for and meet the demand. To fill that gap, the Long-Term Quality Alliance, in partnership with Brandeis University, added supplemental questions to the Behavioral Risk Factor Surveillance System (BRFSS) — a national survey administered by states — to determine disability prevalence and LTSS needs in two states, Washington and Texas. As the Alliance’s Christina Wu and the Commonwealth Fund’s Corinne Lewis report on To the Point, the pilots confirm that BRFSS is an effective vehicle for collecting rich data on LTSS needs of Americans with disabilities.
READ MORE ([link removed] )
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
A roundup of recent Fund publications, charts, multimedia, and other timely content.
Having trouble viewing this email? View online
July 24, 2023
Facebook ([link removed] )
Twitter ([link removed] )
LinkedIn ([link removed] )
The Case for Diversity in Medical Education
The Supreme Court may have struck down race-conscious affirmative action in undergraduate admissions policies, but the case for diversity in medical education and health professions training is as strong as ever, say the Commonwealth Fund’s Laurie Zephyrin, M.D., the National Health Law Program’s Josemiguel Rodriguez, and George Washington University’s Sara Rosenbaum. On To the Point, they cite the overwhelming evidence of racial and ethnic disparities in health and health care as well as research showing that a diverse health care workforce improves access and outcomes, especially for patients of color.
READ MORE ([link removed] )
We Need More Women in Cardiology. Here’s Why.
Forty-four percent of U.S. women now live with some form of heart disease. And although it’s the leading cause of death among women, just 14 percent of cardiologists are women. On The Dose podcast, Joel Bervell interviews cardiologist Martha Gulati, M.D., associate director of the Barbra Streisand Women’s Heart Center at Cedars-Sinai Heart Institute in Los Angeles. She talks about women’s historical exclusion from clinical trials for heart disease, why sex and gender matter in the search for better treatments, and the persistent gaps in women’s cardiology care and research — especially related to women of color.
LISTEN NOW ([link removed] )
FEATURED CHART
Value-Based Payment Can Lower Drug Spending
Policymakers have proposed several ways to control drug costs. One promising but largely untried approach is value-based payment, or VBP, which ties payment for health services to their relative cost and efficacy. Experts from the Duke-Margolis Center for Health Policy explore the promise of VBP to “ensure the right drug is used for the right patient at the right time” and to expand access for underserved patients. Among the options available to Medicare, Medicaid, and other health care payers are incentivizing use of low-cost, generic drugs for chronic condition management and helping health care organizations engage specialty clinicians about the drugs they are prescribing, the authors say.
READ MORE ([link removed] )
The Maldives Reduced Maternal Mortality by 90 Percent
In 1990, a staggering 677 women in the Maldives died of pregnancy-related complications for every 100,000 live births. But, as the Commonwealth Fund’s Munira Gunja notes in International Insights, by 2017 the government there had brought that number down to 46 deaths per 100,000 — the world’s largest drop in maternal mortality in the past three decades. The progress made in the Maldives tells us that a concurrent rise in maternal deaths in the U.S. was avoidable. Gunja says that ensuring equitable access to care and having a well-staffed maternal health system are critical factors in reducing maternal mortality.
READ MORE ([link removed] )
Keeping Children on Medicaid During Redeterminations
Millions of children are in danger of losing their coverage under Medicaid as states resume the process of redetermining eligibility now that the COVID-19 public health emergency has ended. On To the Point, the Commonwealth Fund’s Sara Federman and Akeiisa Coleman discuss strategies that states can use to ensure eligible children are not disenrolled for procedural reasons. These include leveraging available data sources to verify eligibility, tailoring outreach and messaging to families with children, and implementing new continuous coverage requirements for children as soon as possible.
READ MORE ([link removed] )
Expanding Access to Mental Health Care
Despite progress, the United States still struggles mightily to ensure everyone can get the mental health services they need. The Biden administration has proposed a series of initiatives to address the crisis, but the reforms require bipartisan congressional approval. Experts from the USC–Brookings Schaeffer Initiative on Health Policy outline steps the federal government can take immediately, under existing authority, to address the nation’s mental health challenges. These include expanding coverage of crisis services across payers and holding public insurance plans accountable for treatment access.
READ MORE ([link removed] )
How Hospitals Can Confront Racism
This month, the Lown Institute published its rankings of the most socially responsible hospitals ([link removed] ) in the country. The rankings assess hospitals on measures of health equity, value, and health outcomes. In a Transforming Care feature examining what health care organizations can do to confront racism ([link removed] ) , we explore nascent efforts led by Lown and others to hold health systems accountable for advancing health equity in their institutions and communities.
Medicaid Takes Aim at Greenhouse Gas Emissions
State Medicaid programs may be poised to become pioneers in reducing greenhouse gas emissions, a shift that could help pave the way to a more sustainable and resilient health care system. On To the Point, Mathematica researchers say that states can leverage their Medicaid programs’ substantial purchasing and regulatory powers to reduce greenhouse gas emissions and address beneficiaries' needs. Several states are developing climate action plans to safeguard residents’ health, while others are scrutinizing their supply chains for ways to reduce carbon emissions.
READ MORE ([link removed] )
Protecting Public Health Requires Bipartisanship
Noting that public health emergencies like COVID-19 “don't discriminate by party affiliation,” two policy experts are urging Congress to bolster the nation’s preparedness by reauthorizing the soon-to-expire Pandemic and All-Hazards Preparedness Act. In their opinion piece for Medpage Today, the Commonwealth Fund’s Rachel Nuzum and the Bipartisan Policy Center’s Anand Parekh, M.D., say that with U.S. health and security at stake, support for the law’s reauthorization, as well as for other measures to enhance emergency readiness, must come from both sides of the political aisle.
READ MORE ([link removed] )
LTSS Needs for Working-Age Adults with Disabilities
Many working-age adults with disabilities need long-term services and supports (LTSS) for help with daily activities such as bathing, preparing meals, and managing medications. Although these needs are expected to grow over the next two decades, federal and state policymakers don’t have the data to plan for and meet the demand. To fill that gap, the Long-Term Quality Alliance, in partnership with Brandeis University, added supplemental questions to the Behavioral Risk Factor Surveillance System (BRFSS) — a national survey administered by states — to determine disability prevalence and LTSS needs in two states, Washington and Texas. As the Alliance’s Christina Wu and the Commonwealth Fund’s Corinne Lewis report on To the Point, the pilots confirm that BRFSS is an effective vehicle for collecting rich data on LTSS needs of Americans with disabilities.
READ MORE ([link removed] )
Affordable, quality health care. For everyone.
The Commonwealth Fund, 1 East 75th Street, New York, NY 10021
Unsubscribe ([link removed] )
Manage preferences ([link removed] )
Message Analysis
- Sender: Commonwealth Fund
- Political Party: n/a
- Country: United States
- State/Locality: n/a
- Office: n/a
-
Email Providers:
- HubSpot
