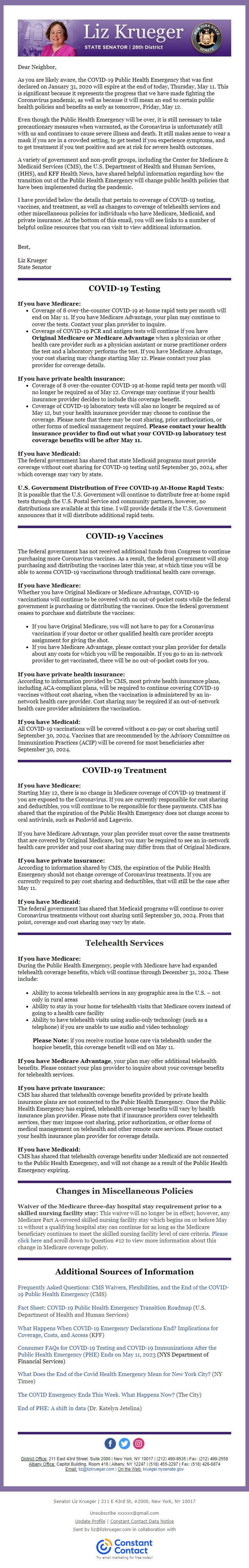
| From | Senator Liz Krueger <[email protected]> |
| Subject | The End of the Public Health Emergency |
| Date | May 11, 2023 4:17 PM |
Links have been removed from this email. Learn more in the FAQ.
Links have been removed from this email. Learn more in the FAQ.
Changes in Public Health Policies Dear Neighbor, As you are likely aware, the COVID-19 Public Health Emergency that was first declared on January 31, 2020 will expire at the end of today, Thursday, May 11. This is significant because it represents the progress that we have made fighting the Coronavirus pandemic, as well as because it will mean an end to certain public health policies and benefits as early as tomorrow, Friday, May 12. Even though the Public Health Emergency will be over, it is still necessary to take precautionary measures when warranted, as the Coronavirus is unfortunately still with us and continues to cause severe illness and death. It still makes sense to wear a mask if you are in a crowded setting, to get tested if you experience symptoms, and to get treatment if you test positive and are at risk for severe health outcomes. A variety of government and non-profit groups, including the Center for Medicare & Medicaid Services (CMS), the U.S. Department of Health and Human Services, (HHS), and KFF Health News, have shared helpful information regarding how the transition out of the Public Health Emergency will change public health policies that have been implemented during the pandemic. I have provided below the details that pertain to coverage of COVID-19 testing, vaccines, and treatment, as well as changes to coverage of telehealth services and other miscellaneous policies for individuals who have Medicare, Medicaid, and private insurance. At the bottom of this email, you will see links to a number of helpful online resources that you can visit to view additional information. Best, Liz Krueger State Senator COVID-19 Testing If you have Medicare: Coverage of 8 over-the-counter COVID-19 at-home rapid tests per month will end on May 11. If you have Medicare Advantage, your plan may continue to cover the tests. Contact your plan provider to inquire. Coverage of COVID-19 PCR and antigen tests will continue if you have Original Medicare or Medicare Advantage when a physician or other health care provider such as a physician assistant or nurse practitioner orders the test and a laboratory performs the test. If you have Medicare Advantage, your cost sharing may change starting May 12. Please contact your plan provider for coverage details. If you have private health insurance: Coverage of 8 over-the-counter COVID-19 at-home rapid tests per month will no longer be required as of May 12. Coverage may continue if your health insurance provider decides to include this coverage benefit. Coverage of COVID-19 laboratory tests will also no longer be required as of May 12, but your health insurance provider may choose to continue the coverage. Please note that there may be cost sharing, prior authorization, or other forms of medical management required. Please contact your health insurance provider to find out what your COVID-19 laboratory test coverage benefits will be after May 11. If you have Medicaid: The federal government has shared that state Medicaid programs must provide coverage without cost sharing for COVID-19 testing until September 30, 2024, after which coverage may vary by state. U.S. Government Distribution of Free COVID-19 At-Home Rapid Tests: It is possible that the U.S. Government will continue to distribute free at-home rapid tests through the U.S. Postal Service and community partners, however, no distributions are available at this time. I will provide details if the U.S. Government announces that it will distribute additional rapid tests. COVID-19 Vaccines The federal government has not received additional funds from Congress to continue purchasing more Coronavirus vaccines. As a result, the federal government will stop purchasing and distributing the vaccines later this year, at which time you will be able to access COVID-19 vaccinations through traditional health care coverage. If you have Medicare: Whether you have Original Medicare or Medicare Advantage, COVID-19 vaccinations will continue to be covered with no out-of-pocket costs while the federal government is purchasing or distributing the vaccines. Once the federal government ceases to purchase and distribute the vaccines: If you have Original Medicare, you will not have to pay for a Coronavirus vaccination if your doctor or other qualified health care provider accepts assignment for giving the shot. If you have Medicare Advantage, please contact your plan provider for details about any costs for which you will be responsible. If you go to an in-network provider to get vaccinated, there will be no out-of-pocket costs for you. If you have private health insurance: According to information provided by CMS, most private health insurance plans, including ACA-compliant plans, will be required to continue covering COVID-19 vaccines without cost sharing, when the vaccination is administered by an in-network health care provider. Cost sharing may be required if an out-of-network health care provider administers the vaccination. If you have Medicaid: All COVID-19 vaccinations will be covered without a co-pay or cost sharing until September 30, 2024. Vaccines that are recommended by the Advisory Committee on Immunization Practices (ACIP) will be covered for most beneficiaries after September 30, 2024. COVID-19 Treatment If you have Medicare: Starting May 12, there is no change in Medicare coverage of COVID-19 treatment if you are exposed to the Coronavirus. If you are currently responsible for cost sharing and deductibles, you will continue to be responsible for these payments. CMS has shared that the expiration of the Public Health Emergency does not change access to oral antivirals, such as Paxlovid and Lagevrio. If you have Medicare Advantage, your plan provider must cover the same treatments that are covered by Original Medicare, but you may be required to see an in-network health care provider and your cost sharing may differ from that of Original Medicare. If you have private insurance: According to information shared by CMS, the expiration of the Public Health Emergency should not change coverage of Coronavirus treatments. If you are currently required to pay cost sharing and deductibles, that will still be the case after May 11. If you have Medicaid: The federal government has shared that Medicaid programs will continue to cover Coronavirus treatments without cost sharing until September 30, 2024. From that point, coverage and cost sharing may vary by state. Telehealth Services If you have Medicare: During the Public Health Emergency, people with Medicare have had expanded telehealth coverage benefits, which will continue through December 31, 2024. These include: Ability to access telehealth services in any geographic area in the U.S. – not only in rural areas Ability to stay in your home for telehealth visits that Medicare covers instead of going to a health care facility Ability to have telehealth visits using audio-only technology (such as a telephone) if you are unable to use audio and video technology Please Note: if you receive routine home care via telehealth under the hospice benefit, this coverage benefit will end on May 11. If you have Medicare Advantage, your plan may offer additional telehealth benefits. Please contact your plan provider to inquire about your coverage benefits for telehealth services. If you have private insurance: CMS has shared that telehealth coverage benefits provided by private health insurance plans are not connected to the Pubic Health Emergency. Once the Public Health Emergency has expired, telehealth coverage benefits will vary by health insurance plan provider. Please note that if insurance providers cover telehealth services, they may impose cost sharing, prior authorization, or other forms of medical management on telehealth and other remote care services. Please contact your health insurance plan provider for coverage details. If you have Medicaid: CMS has shared that telehealth coverage benefits under Medicaid are not connected to the Public Health Emergency, and will not change as a result of the Public Health Emergency expiring. Changes in Miscellaneous Policies Waiver of the Medicare three-day hospital stay requirement prior to a skilled nursing facility stay: This waiver will no longer be in effect; however, any Medicare Part A-covered skilled nursing facility stay which begins on or before May 11 without a qualifying hospital stay can continue for as long as the Medicare beneficiary continues to meet the skilled nursing facility level of care criteria. Please click here and scroll down to Question #12 to view more information about this change in Medicare coverage policy. Additional Sources of Information Frequently Asked Questions: CMS Waivers, Flexibilities, and the End of the COVID-19 Public Health Emergency (CMS) Fact Sheet: COVID-19 Public Health Emergency Transition Roadmap (U.S. Department of Health and Human Services) What Happens When COVID-19 Emergency Declarations End? Implications for Coverage, Costs, and Access (KFF) Consumer FAQs for COVID-19 Testing and COVID-19 Immunizations After the Public Health Emergency (PHE) Ends on May 11, 2023 (NYS Department of Financial Services) What Does the End of the Covid Health Emergency Mean for New York City? (NY Times) The COVID Emergency Ends This Week. What Happens Now? (The City) End of PHE: A shift in data (Dr. Katelyn Jetelina) District Office: 211 East 43rd Street, Suite 2000 | New York, NY 10017 | (212) 490-9535 | Fax: (212) 499-2558 Albany Office: Capitol Building, Room 416 | Albany, NY 12247 | (518) 455-2297 | Fax: (518) 426-6874 Email: [email protected] | On the Web: krueger.nysenate.gov Senator Liz Krueger | 211 E 43rd St, #2000, New York, NY 10017 Unsubscribe [email protected] Update Profile | Constant Contact Data Notice Sent by [email protected] in collaboration with Try email marketing for free today!
Message Analysis
- Sender: Liz Krueger
- Political Party: Democratic
- Country: United States
- State/Locality: New York
- Office: State Senate
-
Email Providers:
- Constant Contact
